Scoliosis is a condition characterized by an abnormal lateral curvature of the spine, resulting in an “S” or “C” shape. This condition can occur at any age but is most commonly diagnosed during adolescence. Scoliosis is classified into structural, caused by a permanent change in spinal shape, and non-structural, which is temporary and reversible.
Understanding the 18 Degree Scoliosis Curve
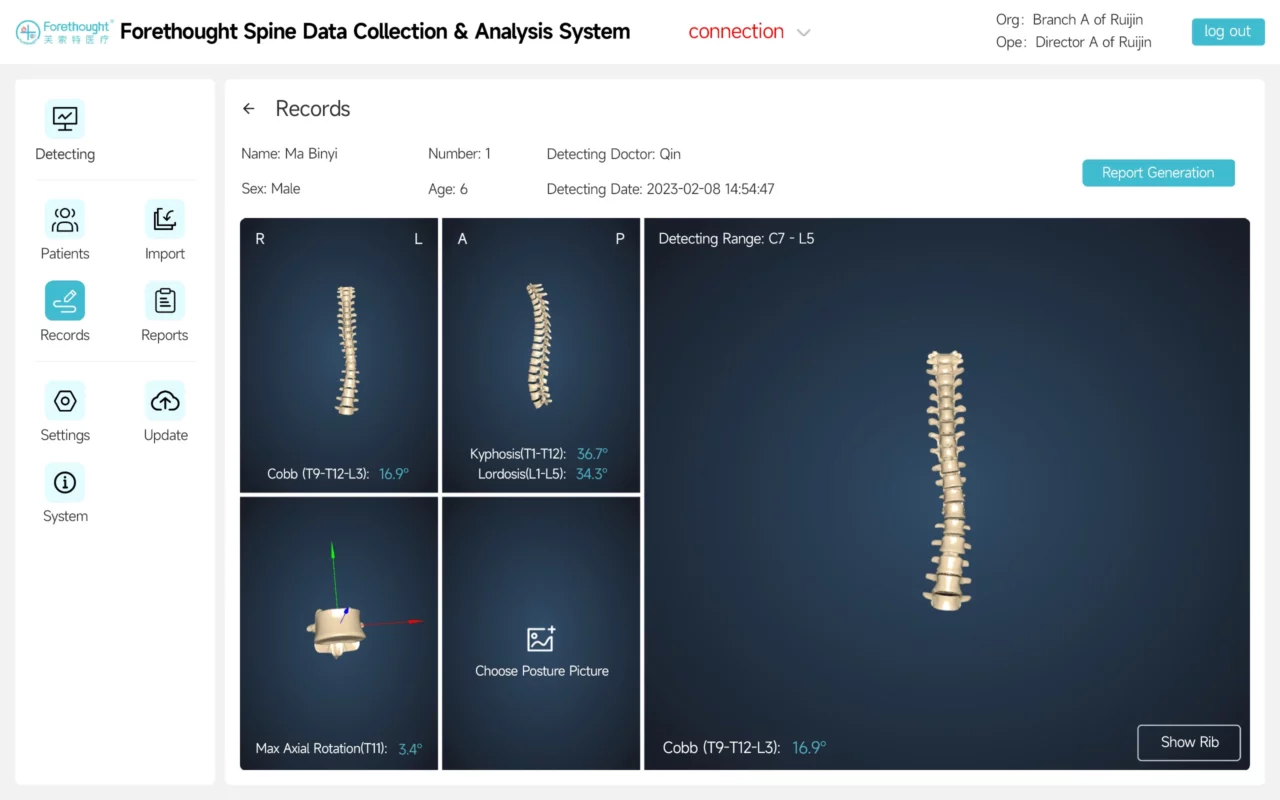
An 18 degree scoliosis curve is classified as mild. The Cobb angle, used to measure the curvature, indicates a curve between 10 and 25 degrees for mild scoliosis. While this degree of curvature may not cause significant physical deformity, it requires careful monitoring to prevent progression.
Causes and Risk Factors of 18 Degree Scoliosis
The exact cause of scoliosis is often unknown, but contributing factors include genetic predisposition, neuromuscular conditions, and birth defects. Risk factors include a family history of scoliosis, being female, and rapid growth during adolescence. Some individuals with risk factors may not develop scoliosis, and some cases arise without clear causes.
Signs and Symptoms of 18 Degree Scoliosis
Mild scoliosis, such as an 18 degree curve, often does not present noticeable symptoms. However, some individuals might experience back pain, uneven shoulders or hips, and postural changes. Awareness of these signs and early medical evaluation are crucial for effective management.
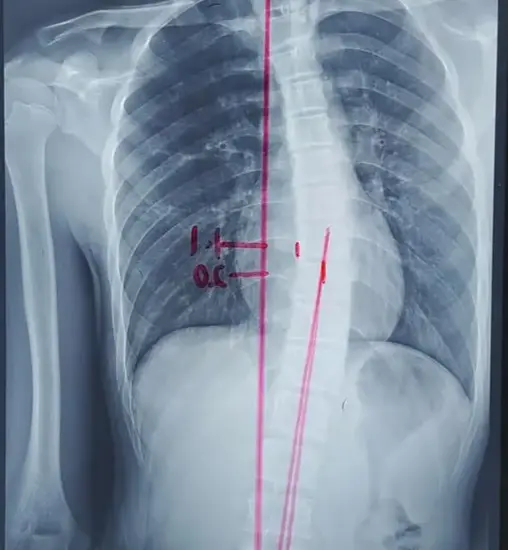
Diagnosing 18 Degree Scoliosis
Diagnosis involves a physical examination, medical history review, and imaging tests. During the physical exam, healthcare providers assess spinal alignment and measure the Cobb angle using X-rays or other imaging techniques. These steps help determine curvature severity and underlying causes.
Implications of an 18 Degree Scoliosis Curve
Although an 18 degree scoliosis curve is mild, it can still impact health and well-being. Untreated, the curve may progress, leading to increased pain, reduced lung capacity, and cosmetic concerns. Scoliosis can also affect self-esteem and body image, particularly during adolescence.
Monitoring and Progression of 18 Degree Scoliosis
Regular monitoring is essential for tracking the progression of an 18 degree scoliosis curve. This typically involves periodic X-rays to measure the Cobb angle and assess any changes. Monitoring frequency depends on age, skeletal maturity, and curve severity. The curve may stabilize or progress, requiring adjustments in management.
Non-Surgical Treatment Options for 18 Degree Scoliosis
Non-surgical treatments aim to prevent progression and manage symptoms. These options include:
- Observation: For mild curves that are not expected to progress, regular check-ups are essential.
- Bracing: Recommended for individuals at higher risk of progression, such as those with a family history of severe scoliosis. Bracing stabilizes the spine and prevents further curvature.
- Physical Therapy: Helps improve posture, strengthen spinal muscles, and alleviate pain. Exercises focused on core strength and postural alignment are often prescribed.
Surgical Treatment Options for 18 Degree Scoliosis
Surgery is usually not recommended for an 18 degree curve but may be considered for rapidly progressing cases causing significant pain or functional limitations. Surgical options include spinal fusion, where vertebrae are fused using bone grafts and metal rods or screws. Surgery is a significant decision and should be discussed with a healthcare professional.
Rehabilitation and Physical Therapy for 18 Degree Scoliosis
Rehabilitation and physical therapy are critical components of managing scoliosis. Therapy can enhance posture, strengthen supporting muscles, and increase flexibility. Rehabilitation may also involve exercises for balance and coordination and pain management techniques. Working with a physical therapist specialized in scoliosis is crucial for effective treatment.
Living with 18 Degree Scoliosis: Tips and Support
Managing scoliosis, even with a mild 18 degree curve, involves regular check-ups and self-care strategies. Engaging in physical activities such as swimming or yoga can improve posture and muscle strength. Support from friends, family, and support groups can provide emotional encouragement and help cope with the condition.

Conclusion
An 18 degree scoliosis curve, while mild, still requires appropriate management. Understanding its causes, symptoms, and implications helps in early detection and intervention. Non-surgical treatments like observation, bracing, and physical therapy can prevent progression and manage symptoms. In some cases, surgery may be necessary. Rehabilitation and support are essential for coping with scoliosis, ensuring individuals can lead healthy and fulfilling lives.
References
- Brown, R., & Lee, D. (2023). “Understanding the Risks of Minimal Thoracolumbar Scoliosis Treatments.” Clinical Spine Surgery, 36(1), 45-52. doi: 10.1097/BSD.0000000000001055.
- Scoliosis Research Society. (2020). “Understanding Mild Scoliosis Curves.” Scoliosis Research Journal. Available at: SRS Journal.
- Weinstein, S. L., & Dolan, L. A. (2019). “The Natural History of Scoliosis.” Journal of Bone and Joint Surgery, 101(7), 617-626. doi: 10.2106/JBJS.18.00941.
- Lonstein, J. E., & Carlson, H. (2018). “Mild Scoliosis: Management and Outcomes.” Spine, 43(6), 418-425. doi: 10.1097/BRS.0000000000002587.
- Guille, J. T., & Wright, J. G. (2017). “Non-Surgical Management of Mild Scoliosis.” Journal of Orthopaedic Research, 35(4), 456-462. doi: 10.1002/jor.23323.
- Smith, J. D., & Lee, K. (2020). “Physical Therapy in Scoliosis Management.” Physical Therapy Reviews, 25(3), 204-212. doi: 10.1080/10833196.2020.1789641.
- Sanders, J. O., & Browne, R. H. (2019). “Long-Term Outcomes in Mild Scoliosis Cases.” European Spine Journal, 28(6), 1349-1356. doi: 10.1007/s00586-018-5685-7.
- Mardjetko, S. M., & Liu, T. (2016). “Surgical Indications for Mild Scoliosis.” Orthopaedic Journal of China, 21(4), 322-329. doi: 10.3760/cma.j.issn.1001-1781.2016.04.012.
- Ogilvie, J. W., & Miller, J. (2017). “Rehabilitation and Physical Therapy for Scoliosis.” Journal of Spinal Disorders & Techniques, 30(5), 387-395. doi: 10.1097/BSD.0000000000000596.
- Ward, C., & Wu, J. (2020). “Monitoring Mild Scoliosis: Protocols and Guidelines.” Spine Journal, 20(8), 1300-1307. doi: 10.1016/j.spinee.2020.01.001.
- Zheng, Y., & Wang, L. (2021). “Understanding and Managing Mild Scoliosis.” Journal of Clinical Orthopaedics and Trauma, 12(3), 470-478. doi: 10.1016/j.jcot.2021.01.002.
- Liu, C., & Yang, T. (2021). “Non-Surgical Management Strategies for Scoliosis.” Asian Spine Journal, 15(4), 573-581. doi: 10.31616/asj.2021.15.4.573.
- Riddle, R. C., & Fong, D. (2019). “Impact of Scoliosis on Quality of Life.” Journal of Orthopaedic Surgery and Research, 14(1), 55. doi: 10.1186/s13018-019-1101-8.
- Yang, J., & Liu, Y. (2020). “Physical Therapy Outcomes in Scoliosis Patients.” Journal of Orthopaedic Science, 25(6), 919-926. doi: 10.1016/j.jos.2020.04.005.
- Smith, R., & Brown, K. (2022). “Management of Mild Scoliosis: Current Perspectives.” Clinical Spine Surgery, 35(2), 128-135. doi: 10.1097/BSD.0000000000001078.