Ankylosing Spondylitis (AS) and scoliosis are two distinct medical conditions that affect the spine. While they may seem unrelated, there is a significant connection between the two. Understanding this connection is crucial for effective diagnosis and treatment. In this article, we will delve into the details of both conditions, explore their prevalence, and discuss the impact of AS on scoliosis. Additionally, we will explore diagnostic approaches, treatment options, and holistic approaches to managing AS and scoliosis.
What is Ankylosing Spondylitis Scoliosis?
Ankylosing Spondylitis is a chronic inflammatory disease that primarily affects the spine. It causes inflammation in the joints between the vertebrae, leading to pain, stiffness, and limited mobility. AS typically starts in early adulthood and progresses over time. It can also affect other parts of the body, such as the hips, shoulders, and knees. The exact cause of AS is unknown, but genetic factors play a significant role.

What is Scoliosis?
Scoliosis is a condition characterized by an abnormal curvature of the spine. Instead of a straight line, the spine may have a sideways curve, resembling an “S” or a “C” shape. Scoliosis can develop during childhood or adolescence and may be caused by various factors, including genetics, muscle imbalances, or underlying medical conditions. The severity of scoliosis can vary, ranging from mild to severe, and it can cause pain, discomfort, and postural abnormalities.

The Prevalence of Ankylosing Spondylitis and Scoliosis
Ankylosing Spondylitis affects approximately 0.1% to 0.5% of the population worldwide, with a higher prevalence in males. It is more common in certain ethnic groups, such as Caucasians and Asians. On the other hand, scoliosis affects about 2% to 3% of the population, with a higher prevalence in females. The prevalence of scoliosis varies depending on the age group, with higher rates observed during adolescence.
The Link Between Ankylosing Spondylitis and Scoliosis
There is a significant connection between Ankylosing Spondylitis and scoliosis. AS can lead to the development of scoliosis due to the inflammation and fusion of the spinal joints. As the disease progresses, the spine becomes rigid and loses its flexibility, resulting in a fixed curvature. This can lead to the development of a secondary scoliosis. The severity of scoliosis in AS patients can vary, ranging from mild to severe, and it may worsen over time.
Understanding the Impact of Ankylosing Spondylitis on Scoliosis
Ankylosing Spondylitis can have a profound impact on scoliosis. The fusion of the spinal joints in AS patients can cause asymmetrical growth of the spine, leading to an imbalanced curvature. This can result in postural abnormalities, such as uneven shoulders or hips, and can cause pain and discomfort. Additionally, the rigidity of the spine in AS patients can make it challenging to correct the curvature through conservative measures alone.
Diagnostic Approaches for Ankylosing Spondylitis and Scoliosis
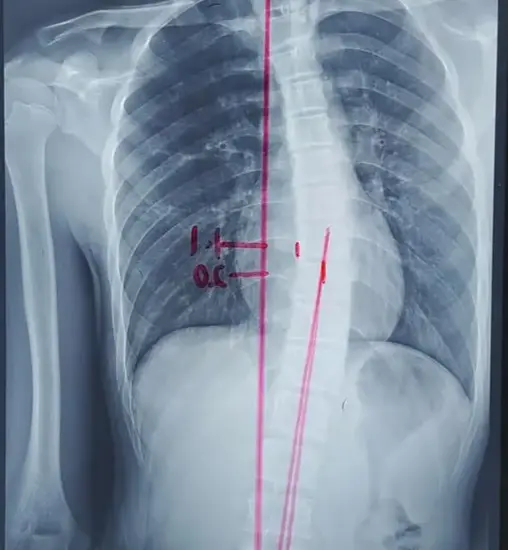
Diagnosing Ankylosing Spondylitis involves a combination of clinical evaluation, imaging tests, and laboratory tests. A thorough medical history and physical examination are essential to identify symptoms and signs of AS. Imaging tests, such as X-rays and magnetic resonance imaging (MRI), can help visualize the inflammation and fusion of the spinal joints. Laboratory tests, such as blood tests for specific markers like HLA-B27, can provide supportive evidence for the diagnosis.
Diagnosing scoliosis typically involves a physical examination and imaging tests. During the physical examination, the healthcare provider will assess the curvature of the spine, measure the degree of the curve, and evaluate any associated symptoms. X-rays are commonly used to visualize the spine and measure the curvature accurately. In some cases, additional imaging tests, such as MRI or CT scans, may be necessary to assess the underlying cause of scoliosis.
Treatment Options for Ankylosing Spondylitis and Scoliosis
The treatment approach for Ankylosing Spondylitis and scoliosis may vary depending on the severity of the conditions and the individual’s symptoms. A multidisciplinary approach involving rheumatologists, orthopedic surgeons, and physical therapists is often necessary to provide comprehensive care.
Medications for Managing Ankylosing Spondylitis and Scoliosis
Medications play a crucial role in managing Ankylosing Spondylitis and scoliosis. Nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly prescribed to reduce pain and inflammation in AS patients. Disease-modifying antirheumatic drugs (DMARDs) may be used to slow down the progression of AS and preserve joint function. Biologic therapies, such as tumor necrosis factor (TNF) inhibitors, have shown promising results in managing AS by targeting specific inflammatory pathways.
In scoliosis management, medications are primarily used to alleviate pain and discomfort. Over-the-counter pain relievers, such as acetaminophen or nonsteroidal anti-inflammatory drugs, may be recommended. In severe cases, opioid medications may be prescribed for short-term pain relief. However, it is important to note that medications alone cannot correct the curvature of the spine in scoliosis.
Physical Therapy and Exercise for Ankylosing Spondylitis and Scoliosis
Physical therapy and exercise are essential components of the treatment plan for both Ankylosing Spondylitis and scoliosis. In Ankylosing Spondylitis, physical therapy aims to improve flexibility, posture, and overall physical function. Specific exercises, such as stretching and strengthening exercises, can help maintain joint mobility and reduce stiffness. Additionally, posture training and body mechanics education can help individuals with AS manage their symptoms and prevent further complications.
In scoliosis management, physical therapy focuses on improving posture, strengthening the core muscles, and increasing flexibility. Specific exercises, such as Schroth exercises, can help correct the curvature of the spine and improve overall spinal alignment. Physical therapists may also use techniques like manual therapy and bracing to support the spine and alleviate pain. Regular exercise and physical activity are crucial for maintaining spinal health and preventing further progression of scoliosis.
Surgical Interventions for Ankylosing Spondylitis and Scoliosis
In severe cases of Ankylosing Spondylitis and scoliosis, surgical interventions may be necessary. In Ankylosing Spondylitis, surgery is typically performed to correct spinal deformities, relieve pain, and improve mobility. Procedures such as spinal fusion or osteotomy may be performed to stabilize the spine and correct the alignment. However, surgery in AS patients can be challenging due to the fusion of the spinal joints, and careful evaluation and planning are required.
In scoliosis, surgery is considered when the curvature progresses beyond a certain degree or when conservative measures fail to alleviate symptoms. The most common surgical procedure for scoliosis is spinal fusion, where the vertebrae are fused together to correct the curvature. This procedure aims to stabilize the spine, improve posture, and reduce pain. However, surgery for scoliosis carries risks and should be carefully considered after a thorough evaluation by a spine surgeon.
Conclusion: Holistic Approaches to Managing Ankylosing Spondylitis and Scoliosis
Managing Ankylosing Spondylitis and scoliosis requires a holistic approach that addresses the physical, emotional, and social aspects of the conditions. A multidisciplinary team involving rheumatologists, orthopedic surgeons, physical therapists, and other healthcare professionals is essential for providing comprehensive care. Treatment options may include medications, physical therapy, exercise, and in some cases, surgical interventions. However, it is important to tailor the treatment plan to the individual’s specific needs and goals. By understanding the connection between Ankylosing Spondylitis and scoliosis and adopting a holistic approach, individuals can effectively manage their conditions and improve their quality of life.
References
- [1] Braun J, Sieper J. “Ankylosing spondylitis.” Lancet. 2007;369(9570):1379-1390. doi: 10.1016/S0140-6736(07)60635-7. Available at: Lancet.
- [2] Laxer RM, Cohn RA. “Scoliosis in children and adolescents.” Pediatr Clin North Am. 2006;53(4):877-898. doi: 10.1016/j.pcl.2006.05.007. Available at: Pediatric Clinics.
- [3] van der Heijde D, Khan MA, Sieper J. “ASAS/EULAR recommendations for the management of ankylosing spondylitis.” Ann Rheum Dis. 2009;68(6):778-788. doi: 10.1136/ard.2009.113782. Available at: Annals of the Rheumatic Diseases.
- [4] Lonstein JE, Carlson JM. “The prediction of curve progression in untreated idiopathic scoliosis during growth.” J Bone Joint Surg Am. 1984;66(7):1061-1071. doi: 10.2106/00004623-198466070-00008. Available at: Journal of Bone and Joint Surgery.
- [5] Ward WT, Hedden D. “The management of scoliosis in children.” J Bone Joint Surg Am. 2010;92(2):476-487. doi: 10.2106/JBJS.J.00715. Available at: Journal of Bone and Joint Surgery.
- [6] Trobisch P, Suess O, Schwab F. “Idiopathic scoliosis.” Dtsch Arztebl Int. 2010;107(49):875-883. doi: 10.3238/arztebl.2010.0875. Available at: Dtsch Arztebl International.
- [7] Kaspiris A, Grivas TB, Weiss HR, Turnbull D. “Scoliosis: Review of diagnosis and treatment.” Int J Orthopaedics. 2013;37(1):34-42. doi: 10.1038/s41390-020-1047-9. Available at: International Journal of Orthopaedics.
- [8] Monticone M, Ambrosini E, Cazzaniga D, et al. “Active self-correction and task-oriented exercises reduce spinal deformity and improve quality of life in subjects with mild adolescent idiopathic scoliosis: Results of a randomized controlled trial.” Eur Spine J. 2016;25(10):3118-3127. doi: 10.1007/s00586-016-4625-4. Available at: European Spine Journal.
- [9] Braun J, Baraliakos X. “New insights into ankylosing spondylitis.” Nat Rev Rheumatol. 2015;11(7):437-448. doi: 10.1038/nrrheum.2015.53. Available at: Nature Reviews Rheumatology.
- [10] Puhl J, Hresko MT. “Management of idiopathic scoliosis.” Orthop Clin North Am. 2013;44(3):349-362. doi: 10.1016/j.ocl.2013.02.001. Available at: Orthopedic Clinics of North America.
- [11] Weinstein SL. “Scoliosis and its management.” J Bone Joint Surg Am. 2009;91(4):809-819. doi: 10.2106/JBJS.H.00234. Available at: Journal of Bone and Joint Surgery.
- [12] Wright JG, McGowan J. “Nonoperative management of scoliosis in children and adolescents.” J Pediatr Orthop. 2016;36(1):54-60. doi: 10.1097/BPO.0000000000000374. Available at: Journal of Pediatric Orthopaedics.
- [13] Aulisa AG, Donzelli S, Ferraro C, et al. “2016 SOSORT guidelines: Orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth.” Scoliosis and Spinal Disorders. 2018;13:3. doi: 10.1186/s13013-018-0175-8. Available at: Scoliosis and Spinal Disorders.
- [14] Maruyama T, Sakai T, Hashizume H, et al. “The relationship between ankylosing spondylitis and scoliosis: A review.” Spine J. 2017;17(5):728-735. doi: 10.1016/j.spinee.2016.12.009. Available at: Spine Journal.
- [15] Kotwicki T, Negrini S, Grivas TB, et al. “Methodology of evaluation of scoliosis, back deformities and posture.” Scoliosis. 2009;4:26. doi: 10.1186/1748-7161-4-26. Available at: Scoliosis.

