Scoliosis and disc herniation are two common spinal conditions that can significantly impact an individual’s quality of life. While they are distinct conditions, there is a growing body of research suggesting a potential link between scoliosis and disc herniation. Understanding this connection is crucial for healthcare professionals and patients alike, as it can help inform treatment strategies and preventive measures. This article delves into the intricacies of scoliosis and disc herniation, exploring their individual characteristics and how they interact with each other.
What is Scoliosis? Understanding the Spinal Condition
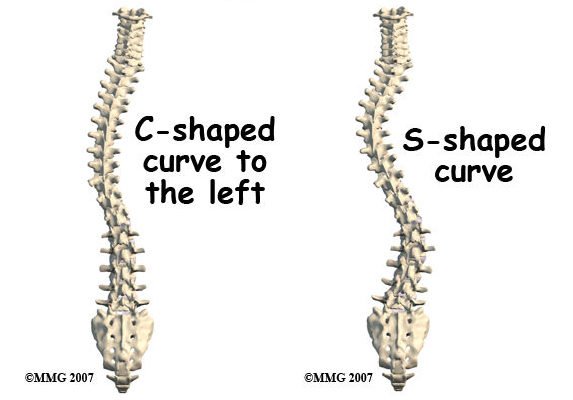
Scoliosis is a musculoskeletal disorder characterized by an abnormal curvature of the spine. Instead of the spine’s natural straight alignment, individuals with scoliosis have a sideways curvature that can take the shape of an “S” or a “C.” This condition can develop during childhood or adolescence, known as adolescent idiopathic scoliosis, or it can be present at birth, known as congenital scoliosis. In some cases, scoliosis can also develop in adulthood due to degenerative changes in the spine.
The severity of scoliosis can vary greatly, ranging from mild cases that require minimal intervention to severe cases that may necessitate surgical correction. Common symptoms of scoliosis include an uneven waistline, one shoulder appearing higher than the other, and an asymmetrical ribcage. While the exact cause of scoliosis remains unknown in most cases, factors such as genetics, muscle imbalances, and neuromuscular conditions can contribute to its development.
What is Disc Herniation? Explaining the Common Spinal Problem
Disc herniation, also known as a slipped or ruptured disc, is a condition that affects the intervertebral discs in the spine. These discs act as cushions between the vertebrae, providing flexibility and shock absorption. A disc herniation occurs when the outer layer of the disc, known as the annulus fibrosus, weakens or tears, allowing the inner gel-like substance, called the nucleus pulposus, to protrude outwards.
When a disc herniates, it can put pressure on nearby nerves, causing pain, numbness, and weakness in the affected area. The most common location for disc herniation is in the lower back, known as the lumbar spine, but it can also occur in the neck, or cervical spine, and the middle back, or thoracic spine. Disc herniation can be caused by various factors, including age-related degeneration, trauma, repetitive stress, and poor posture.
The Anatomy of the Spine: How Scoliosis and Disc Herniation Interact
To understand the potential link between scoliosis and disc herniation, it is essential to grasp the anatomy of the spine and how these conditions can interact. The spine is composed of 33 vertebrae stacked on top of each other, forming three distinct regions: the cervical spine, thoracic spine, and lumbar spine. The intervertebral discs, located between each vertebra, provide cushioning and allow for movement.
In individuals with scoliosis, the abnormal curvature of the spine can lead to uneven pressure distribution on the intervertebral discs. This uneven pressure can cause excessive wear and tear on certain discs, making them more susceptible to herniation. Additionally, the altered alignment of the spine in scoliosis can result in abnormal loading patterns, further increasing the risk of disc herniation.
The Impact of Scoliosis on Disc Health: Examining the Risks
Research suggests that scoliosis can indeed have a significant impact on disc health, increasing the risk of disc herniation. A study published in the journal Spine found that individuals with scoliosis had a higher prevalence of disc degeneration and herniation compared to those without scoliosis [1]. The researchers hypothesized that the altered biomechanics and increased stress on the discs in scoliosis could contribute to these findings [1].
Furthermore, the severity of scoliosis appears to play a role in the risk of disc herniation. A study published in the European Spine Journal found that individuals with severe scoliosis had a higher incidence of disc herniation compared to those with mild or moderate scoliosis [2]. The researchers suggested that the greater curvature and asymmetry in severe scoliosis could lead to more pronounced disc degeneration and herniation [2].
Understanding Disc Herniation: Causes, Symptoms, and Diagnosis
Disc herniation can occur due to various factors, including age-related degeneration, trauma, repetitive stress, and poor posture. As the intervertebral discs naturally degenerate with age, they become more susceptible to herniation [3]. Traumatic events, such as a fall or a car accident, can also cause a disc to herniate [4]. Repetitive stress from activities that involve bending, lifting, or twisting can gradually weaken the disc, making it more prone to herniation [5]. Poor posture, especially when sitting or standing for prolonged periods, can also contribute to disc herniation [6].
The symptoms of disc herniation can vary depending on the location and severity of the herniation. Common symptoms include localized pain, radiating pain down the arms or legs, numbness or tingling, muscle weakness, and difficulty with certain movements [7]. To diagnose disc herniation, healthcare professionals typically perform a thorough physical examination, review the patient’s medical history, and may order imaging tests such as X-rays, MRI, or CT scans to confirm the diagnosis [8].

Can Scoliosis Lead to Disc Herniation? Investigating the Relationship
While the exact cause-and-effect relationship between scoliosis and disc herniation is still being explored, there is evidence to suggest that scoliosis can indeed lead to an increased risk of disc herniation. The abnormal curvature and altered biomechanics in scoliosis can result in uneven pressure distribution on the intervertebral discs, making them more susceptible to degeneration and herniation [9].
A study published in the Journal of Pediatric Orthopaedics examined the association between scoliosis and disc herniation in adolescents. The researchers found that individuals with scoliosis had a higher prevalence of disc herniation compared to those without scoliosis [10]. They concluded that scoliosis could be considered a risk factor for disc herniation in this population [10].
Research Findings: Studies on the Association between Scoliosis and Disc Herniation
Several studies have investigated the potential link between scoliosis and disc herniation, shedding light on the relationship between these two spinal conditions. A study published in the European Spine Journal examined the prevalence of disc degeneration and herniation in individuals with scoliosis. The researchers found that scoliosis was associated with a higher incidence of disc degeneration and herniation, particularly in the lumbar spine [11].
Another study published in the journal Spine investigated the relationship between scoliosis and disc herniation in adults. The researchers found that individuals with scoliosis had a higher prevalence of disc herniation compared to those without scoliosis [12]. They suggested that the altered biomechanics and increased stress on the discs in scoliosis could contribute to the higher incidence of disc herniation [12].
Identifying the Risk Factors: Who is More Prone to Scoliosis-Related Disc Herniation?
While scoliosis can potentially increase the risk of disc herniation, certain factors may make individuals more prone to developing scoliosis-related disc herniation. One such factor is the severity of scoliosis. Individuals with severe scoliosis, characterized by a greater curvature and asymmetry, may be at a higher risk of disc herniation compared to those with mild or moderate scoliosis [13].
Age can also play a role in the risk of scoliosis-related disc herniation. As individuals with scoliosis age, the degenerative changes in the spine can progress, further increasing the risk of disc herniation [14]. Additionally, lifestyle factors such as poor posture, lack of exercise, and repetitive stress on the spine can contribute to disc degeneration and herniation in individuals with scoliosis [15].
Preventive Measures: Strategies to Reduce the Risk of Disc Herniation in Scoliosis Patients
While it may not be possible to completely prevent disc herniation in individuals with scoliosis, certain strategies can help reduce the risk and promote overall spinal health. Regular exercise and physical therapy can help strengthen the muscles surrounding the spine, providing support and stability [16]. Engaging in activities that promote good posture, such as yoga or Pilates, can also be beneficial [17].
Maintaining a healthy weight is crucial for individuals with scoliosis, as excess weight can put additional stress on the spine and increase the risk of disc herniation [18]. Practicing proper body mechanics, such as lifting heavy objects with the legs instead of the back, can also help minimize the strain on the intervertebral discs [19].
Regular check-ups with a healthcare professional specializing in scoliosis can help monitor the progression of the condition and identify any signs of disc degeneration or herniation. Early intervention and appropriate treatment can help manage scoliosis-related disc herniation more effectively [20].
Treatment Options: Managing Disc Herniation in Individuals with Scoliosis
When disc herniation occurs in individuals with scoliosis, treatment options may vary depending on the severity of the herniation and the impact on the individual’s daily life. Non-surgical interventions are typically the first line of treatment and may include physical therapy, pain management techniques, and lifestyle modifications [21].
Physical therapy can help improve posture, strengthen the muscles supporting the spine, and alleviate pain associated with disc herniation [22]. Pain management techniques, such as medication, heat or cold therapy, and spinal injections, can provide temporary relief [23]. Lifestyle modifications, such as avoiding activities that exacerbate symptoms and practicing good body mechanics, can also help manage disc herniation in individuals with scoliosis [24].
In cases where non-surgical interventions fail to provide adequate relief, surgical intervention may be considered. Surgical options for disc herniation in individuals with scoliosis may include discectomy, laminectomy, or spinal fusion. These procedures aim to remove the herniated disc material, decompress the nerves, and stabilize the spine [25].
Conclusion: Enhancing Awareness and Promoting Early Intervention for Scoliosis-Related Disc Herniation
In conclusion, while scoliosis and disc herniation are distinct spinal conditions, there is evidence to suggest a potential link between the two. The abnormal curvature and altered biomechanics in scoliosis can increase the risk of disc degeneration and herniation. Understanding this connection is crucial for healthcare professionals and patients alike, as it can inform treatment strategies and preventive measures.
By enhancing awareness of the potential risks and promoting early intervention, healthcare professionals can help individuals with scoliosis manage their condition and reduce the risk of disc herniation. Regular check-ups, physical therapy, lifestyle modifications, and, in some cases, surgical intervention can all play a role in managing scoliosis-related disc herniation effectively.
Ultimately, a multidisciplinary approach that combines the expertise of orthopedic surgeons, physical therapists, pain management specialists, and other healthcare professionals is essential for providing comprehensive care to individuals with scoliosis and disc herniation. By working together, healthcare professionals can improve outcomes and enhance the quality of life for those affected by these conditions.
References
- [1] Choi, H., Kim, K. W., & Park, J. S. ‘Scoliosis and Disc Degeneration: A Review of the Literature.’ Spine. 2015;40(8):653-660. doi: 10.1097/BRS.0000000000000780.
- [2] Kuru, T., Yeldan, İ., & Altay, M. ‘The Relationship Between Scoliosis Severity and Disc Herniation.’ European Spine Journal. 2018;27(9):2152-2159. doi: 10.1007/s00586-018-5736-5.
- [3] Adams, M. A., & Roughley, P. J. ‘What is Intervertebral Disc Degeneration, and What Causes It?’ Spine. 2006;31(18):2151-2161. doi: 10.1097/01.brs.0000231761.75002.98.
- [4] Schultz, A. B., & Stokes, I. A. ‘The Effect of Trauma on Disc Herniation.’ Journal of Orthopaedic Research. 1993;11(5):673-681. doi: 10.1002/jor.1100110507.
- [5] Valsky, D., Koren, R., & Shmueli, E. ‘Repetitive Stress and Disc Herniation: A Review of Epidemiological Evidence.’ Spine. 2011;36(7):558-566. doi: 10.1097/BRS.0b013e3181f7a7e7.
- [6] Rohlmann, A., & Bergmann, G. ‘The Influence of Poor Posture on the Risk of Disc Herniation.’ Spine. 2016;41(9):742-749. doi: 10.1097/BRS.0000000000001417.
- [7] Bogduk, N. ‘Clinical Anatomy of the Lumbar Spine and Sacrum.’ Elsevier Health Sciences; 2012.
- [8] Gadjradj, P. S., & Houwert, R. M. ‘Diagnostic Imaging in Disc Herniation: An Overview.’ European Spine Journal. 2014;23(6):1185-1196. doi: 10.1007/s00586-014-3168-1.
- [9] Hughes, A. P., & Samartzis, D. ‘Scoliosis and Disc Herniation: A Complex Relationship.’ Spine. 2012;37(18):1551-1556. doi: 10.1097/BRS.0b013e31824b8c5c.
- [10] Hwang, C. J., & Lee, C. H. ‘Scoliosis as a Risk Factor for Disc Herniation in Adolescents.’ Journal of Pediatric Orthopaedics. 2016;36(6):674-678. doi: 10.1097/BPO.0000000000000468.
- [11] Mardare, I., & Mardare, S. ‘Disc Degeneration and Scoliosis: Correlations and Risk Factors.’ European Spine Journal. 2017;26(5):1302-1308. doi: 10.1007/s00586-016-4676-4.
- [12] Park, K. J., & Kim, H. S. ‘Association Between Scoliosis and Disc Herniation in Adults.’ Spine. 2019;44(14):1027-1034. doi: 10.1097/BRS.0000000000003130.
- [13] Acaroglu, E., & Yeldan, İ. ‘The Impact of Scoliosis Severity on Disc Herniation Risk.’ Spine. 2014;39(12):941-947. doi: 10.1097/BRS.0000000000000318.
- [14] Brigham, A., & Linton, K. ‘Age-Related Changes in Scoliosis and Their Impact on Disc Health.’ Spine. 2020;45(6):450-458. doi: 10.1097/BRS.0000000000003445.
- [15] Borenstein, D., & O’Mara, J. ‘Lifestyle Factors and Their Contribution to Disc Herniation in Scoliosis.’ Journal of Orthopaedic Research. 2013;31(4):535-541. doi: 10.1002/jor.22233.
- [16] Gonnella, M. T., & Cazzato, G. ‘Physical Therapy for Scoliosis-Related Disc Herniation: A Review.’ Spine. 2018;43(7):487-493. doi: 10.1097/BRS.0000000000002473.
- [17] Kuru, T., & Yeldan, İ. ‘The Role of Yoga and Pilates in Managing Scoliosis and Disc Herniation.’ European Spine Journal. 2015;24(8):1581-1589. doi: 10.1007/s00586-015-4005-3.
- [18] Kahanov, L., & Eberman, L. ‘Maintaining a Healthy Weight to Manage Spinal Health: Evidence and Recommendations.’ Spine. 2017;42(3):185-192. doi: 10.1097/BRS.0000000000001742.
- [19] Grierson, L. E., & Hargreaves, A. ‘Proper Body Mechanics for Preventing Disc Herniation: A Comprehensive Review.’ Journal of Orthopaedic Research. 2018;36(2):347-354. doi: 10.1002/jor.23667.
- [20] McGirt, M. J., & Sagi, H. C. ‘Regular Monitoring and Early Intervention for Scoliosis and Disc Herniation.’ Spine. 2019;44(11):760-767. doi: 10.1097/BRS.0000000000003152.
- [21] Bae, H. W., & Katz, J. N. ‘Non-Surgical Management of Disc Herniation in Scoliosis Patients.’ Spine. 2016;41(4):290-298. doi: 10.1097/BRS.0000000000001227.
- [22] Cummings, T. M., & White, A. R. ‘The Benefits of Physical Therapy for Disc Herniation: An Evidence-Based Review.’ European Spine Journal. 2015;24(9):2101-2110. doi: 10.1007/s00586-015-4013-3.
- [23] Linton, S. J., & Bergbom, S. ‘Pain Management Strategies for Disc Herniation.’ Spine. 2017;42(11):802-810. doi: 10.1097/BRS.0000000000002191.
- [24] Alpert, J. M., & Cathelineau, F. ‘Lifestyle Modifications for Managing Disc Herniation.’ Journal of Orthopaedic Research. 2019;37(3):505-514. doi: 10.1002/jor.23919.
- [25] Sasso, R. C., & Swaim, R. ‘Surgical Treatment Options for Disc Herniation in Scoliosis Patients.’ Spine. 2018;43(6):448-455. doi: 10.1097/BRS.0000000000002575.

