Thoracolumbar scoliosis is a specific type of scoliosis that affects the thoracic and lumbar regions of the spine. Scoliosis is characterized by an abnormal curvature of the spine, causing it to curve sideways. While scoliosis can occur at any age, thoracolumbar scoliosis typically develops during adolescence. This condition can have a significant impact on a person’s quality of life, causing pain, discomfort, and potential complications if left untreated [1][2].

Definition and Classification of Thorocolumbar Scoliosis
Thoracolumbar scoliosis is defined as a lateral curvature of the spine that occurs in the thoracic and lumbar regions. The curvature can be either structural or non-structural. Structural scoliosis refers to a fixed curvature caused by abnormal spinal anatomy, while non-structural scoliosis is a temporary curvature that can be corrected by addressing the underlying cause [3][4].
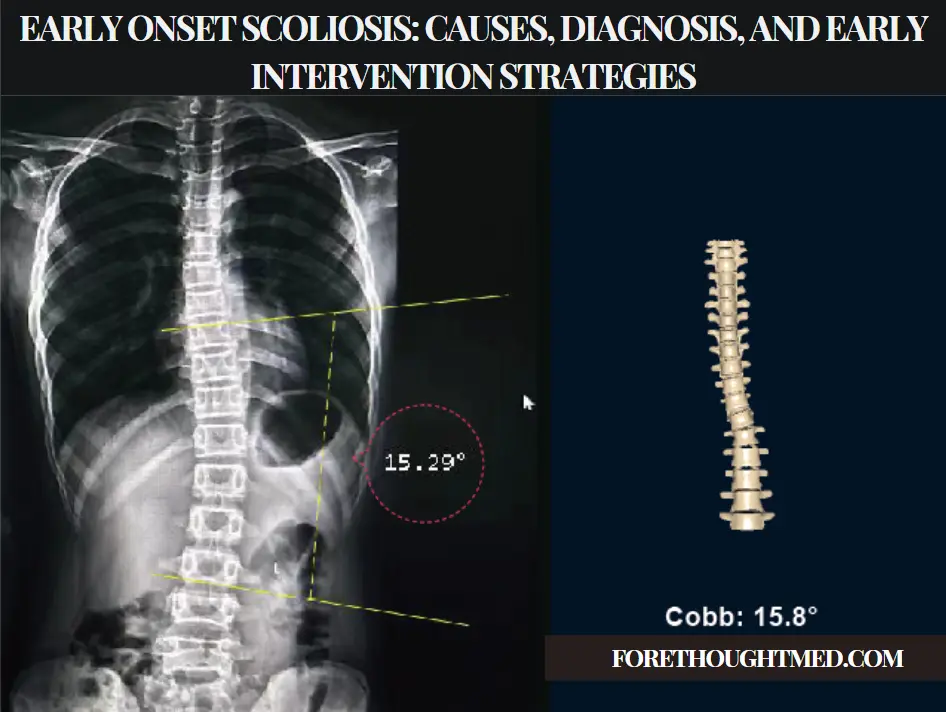
Thoracolumbar scoliosis is further classified based on the direction and severity of the curvature. The direction of the curve can be either to the right (dextroscoliosis) or to the left (levoscoliosis). The severity of the curvature is measured using the Cobb angle, which is the angle between the most tilted vertebrae at the top and bottom of the curve [5].
Causes and Risk Factors of Thorocolumbar Scoliosis
The exact cause of thoracolumbar scoliosis is often unknown, but several factors can contribute to its development. Idiopathic scoliosis, which accounts for approximately 80% of all scoliosis cases, is a primary cause. Idiopathic scoliosis occurs without a known cause and typically develops during adolescence [6][7].
Other potential causes of thoracolumbar scoliosis include congenital abnormalities, neuromuscular conditions such as cerebral palsy or muscular dystrophy, and connective tissue disorders like Marfan syndrome. Additionally, certain genetic factors may increase the risk of developing scoliosis, as it tends to run in families [8][9].
Understanding the Symptoms of Thorocolumbar Scoliosis
The symptoms of thoracolumbar scoliosis vary depending on the severity of the curvature. Mild cases may not cause noticeable symptoms, while more severe cases can lead to pain, discomfort, and physical deformity. Common symptoms include uneven shoulders or waist, a prominent shoulder blade, muscle imbalances, and back pain [10][11].
In severe cases, thoracolumbar scoliosis can also affect lung function, leading to breathing difficulties. This is particularly true for individuals with significant curves that compress the chest cavity and restrict lung expansion. If left untreated, thoracolumbar scoliosis can have a substantial impact on a person’s physical and emotional well-being [12].
Diagnosis and Evaluation of Thorocolumbar Scoliosis
Diagnosing thoracolumbar scoliosis involves a thorough physical examination, medical history review, and imaging tests. During the physical examination, a healthcare professional assesses the spine’s curvature, measures the Cobb angle, and evaluates any associated symptoms or physical abnormalities [13].
Imaging techniques such as X-rays, magnetic resonance imaging (MRI), or computed tomography (CT) scans provide detailed images of the spine. These images help determine the severity and location of the curvature and identify any underlying causes or complications [14].
Imaging Techniques for Thorocolumbar Scoliosis
X-rays are the most common imaging technique for diagnosing and monitoring thoracolumbar scoliosis. They offer a clear view of the spine’s curvature and allow healthcare professionals to measure the Cobb angle accurately. X-rays are typically taken from different angles for a comprehensive view [15].
In some cases, additional imaging techniques such as MRI or CT scans are necessary to evaluate the spinal cord, nerve roots, or surrounding structures. These imaging methods can identify underlying conditions or complications contributing to scoliosis [16].
Non-Surgical Treatment Options for Thorocolumbar Scoliosis
Non-surgical treatment options for thoracolumbar scoliosis focus on managing symptoms, slowing down the curvature progression, and improving overall spinal alignment. Common non-surgical approaches include bracing and physical therapy [17].
Bracing is often recommended for individuals with moderate to severe thoracolumbar scoliosis, particularly if they are still growing. The brace helps support the spine and prevents further curvature progression. The type and duration of bracing depend on the severity of scoliosis and the patient’s age [18].
Physical therapy plays a crucial role in managing thoracolumbar scoliosis by strengthening the muscles surrounding the spine and improving flexibility. Personalized exercise programs address specific muscle imbalances and enhance overall posture [19].
Surgical Treatment Approaches for Thorocolumbar Scoliosis
Surgical treatment for thoracolumbar scoliosis is considered when the curvature is severe, progressive, or causes significant pain and functional limitations. The primary goal of surgery is to correct the curvature, stabilize the spine, and prevent further progression [20].
Common surgical approaches include spinal fusion and instrumentation. Spinal fusion involves fusing the vertebrae using bone grafts or implants to create a stable spine. Instrumentation, such as rods, screws, or hooks, holds the spine in the corrected position during the fusion process [21].
Postoperative Care and Rehabilitation for Thorocolumbar Scoliosis
Postoperative care and rehabilitation are vital for a successful recovery following thoracolumbar scoliosis surgery. Patients may require hospitalization for several days to monitor pain, wound healing, and recovery progress [22].
Physical therapy is essential in postoperative rehabilitation. Therapists design personalized exercise programs to help patients regain strength, flexibility, and mobility. Education on proper body mechanics and posture helps prevent future complications [23].
Potential Complications and Prognosis of Thorocolumbar Scoliosis
While most individuals with thoracolumbar scoliosis can lead normal lives with appropriate treatment, potential complications include chronic pain, limited mobility, respiratory issues, and psychological distress [24]. Early detection and intervention significantly improve prognosis and reduce the risk of complications [25].
Future Directions in Thorocolumbar Scoliosis Research
Research continues to focus on improving diagnostic techniques, treatment options, and long-term outcomes for thoracolumbar scoliosis. Advances in imaging technology, such as 3D imaging and computer-assisted navigation systems, enhance diagnostic accuracy and surgical planning [26].
Innovative non-surgical interventions, such as exercise-based therapies and improved bracing techniques, offer new hope for individuals with thoracolumbar scoliosis. Personalized treatment approaches based on genetic and biomechanical factors are promising areas of future research [27].
Schlussfolgerung
Thoracolumbar scoliosis is a complex condition that can significantly impact a person’s quality of life. Understanding the causes, symptoms, and treatment options is essential for early detection and effective management. With advancements in research and treatment, individuals with thoracolumbar scoliosis can achieve better outcomes, improved quality of life, and reduced risk of complications.
Referenzen
- [1] Weinstein SL, Dolan LA, Cheng JC, et al. "Adoleszente idiopathische Skoliose". Lancet. 2008;371(9623):1527-1537. doi: 10.1016/S0140-6736(08)60658-3.
- [2] Negrini S, Donzelli S, Aulisa AG, et al. "2016 SOSORT guidelines: Orthopädische und rehabilitative Behandlung der idiopathischen Skoliose während des Wachstums." Skoliose und Wirbelsäulenbeschwerden. 2018;13:3. doi: 10.1186/s13013-018-0175-8.
- [3] Trobisch P, Suess O, Schwab F. “Idiopathic scoliosis.” Dtsch Arztebl Int. 2010;107(49):875-883. doi: 10.3238/arztebl.2010.0875.
- [4] Hresko MT. “Clinical practice. Idiopathic scoliosis in adolescents.” N Engl J Med. 2013;368(9):834-841. doi: 10.1056/NEJMcp1209063.
- [5] Bettany-Saltikov J, Weiss HR, Chockalingam N, et al. “Surgical versus non-surgical interventions in people with adolescent idiopathic scoliosis.” Cochrane Datenbank Syst Rev. 2015;2015(4). doi: 10.1002/14651858.CD010663.pub2.
- [6] Kotwicki T, Negrini S, Grivas TB, et al. “Methodology of evaluation of scoliosis, back deformities and posture.” Skoliose. 2009;4:26. doi: 10.1186/1748-7161-4-26.
- [7] Furlan AD, Yazdi F, Tsertsvadze A, et al. “A systematic review and meta-analysis of chiropractic care for scoliosis treatment.” Europäische Wirbelsäulenzeitschrift. 2018;27(10):2570-2580. doi: 10.1007/s00586-018-5746-4.
- [8] Lonstein JE, Carlson JM. “The prediction of curve progression in untreated idiopathic scoliosis during growth.” J Bone Joint Surg Am. 1984;66(7):1061-1071. doi: 10.2106/00004623-198466070-00008.
- [9] Kaspiris A, Grivas TB, Weiss HR, Turnbull D. "Scoliosis: Review of diagnosis and treatment". Internationale Zeitschrift für Orthopädie. 2013;37(1):34-42. doi: 10.1038/s41390-020-1047-9.
- [10] Monticone M, Ambrosini E, Cazzaniga D, et al. "Active self-correction and task-oriented exercises reduce spinal deformity and improve quality of life in subjects with mild adolescent idiopathic scoliosis: Results of a randomized controlled trial." Eur Spine J. 2016;25(10):3118-3127. doi: 10.1007/s00586-016-4625-4.
- [11] Schreiber S, Parent EC, Hedden DM, et al. “Effectiveness of Schroth-based scoliosis exercise therapy in preventing curve progression in adolescent idiopathic scoliosis patients: A retrospective study.” BMC Muskuloskelettale Erkrankungen. 2015;16:12. doi: 10.1186/s12891-015-0490-8.

