Minimal thoracolumbar scoliosis is characterized by a lateral curvature of the spine in the thoracolumbar region measuring less than 20 degrees. This condition, while often mild and asymptomatic, requires proper diagnosis and management to prevent potential complications. This article explores the definition and classification, prevalence and risk factors, clinical presentation, diagnostic evaluation, differential diagnosis, treatment options, prognosis, and potential complications associated with minimal thoracolumbar scoliosis.

Definition and Classification of Minimal Thoracolumbar Scoliosis
Minimal thoracolumbar scoliosis refers to a curvature of the spine less than 20 degrees in the thoracolumbar region, which spans from T10 to L2. It is classified based on the direction of the curve: right thoracolumbar scoliosis and left thoracolumbar scoliosis. Classification helps in guiding treatment decisions by considering the location and severity of the curvature.
Prevalence and Risk Factors
The prevalence of minimal thoracolumbar scoliosis ranges from 2% to 4% in the general population. It is more common in females than males, with a ratio of about 2:1. Typically detected during adolescence due to rapid growth, this condition can also persist into adulthood. Risk factors include genetic predisposition, poor posture, sedentary lifestyle, and certain medical conditions like muscular dystrophy and cerebral palsy.
Clinical Presentation and Symptoms
Most individuals with minimal thoracolumbar scoliosis experience no significant symptoms. Some may report mild back pain or discomfort, particularly after prolonged sitting or standing. Visual asymmetry in the shoulders, waist, or hips may be noticeable. In severe cases, cosmetic concerns or minor impacts on lung function can occur.
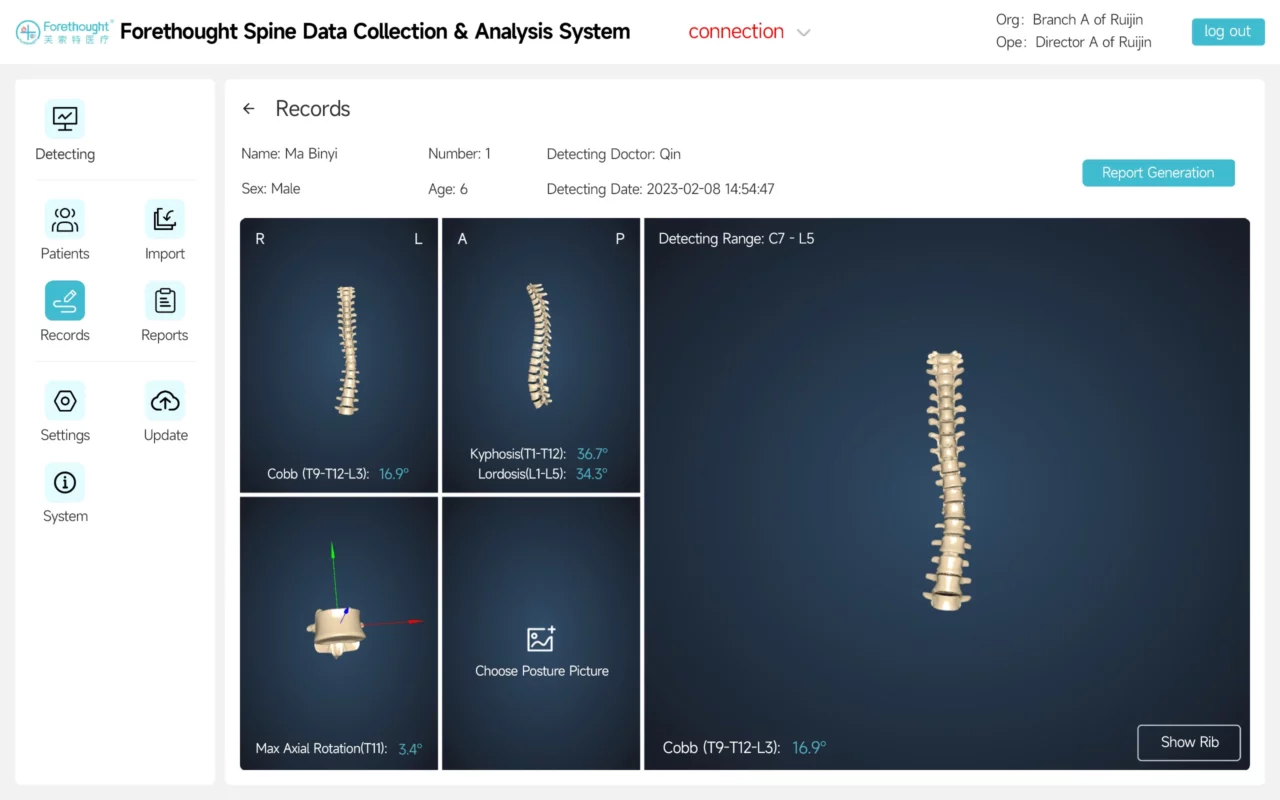
Diagnostic Evaluation and Imaging Techniques
Diagnosis begins with a physical examination, including medical history and assessment of spinal alignment and range of motion. Neurological examination may be performed to check for nerve involvement. Imaging techniques such as X-rays, MRI, or CT scans provide detailed information on curvature severity, location, and associated abnormalities.
Differential Diagnosis
Differential diagnoses for minimal thoracolumbar scoliosis include postural variations, leg length discrepancy, Scheuermann’s disease, and other scoliosis types such as idiopathic or congenital scoliosis. A thorough physical examination and appropriate imaging studies are essential for accurate differentiation.
Treatment Options for Mild Thoracolumbar Scoliosis
Management depends on the curvature severity, symptoms, age, and overall health. Non-surgical approaches are typically preferred, with surgery considered for severe or progressive cases.
Non-Surgical Management Approaches
- Observation and Monitoring: For curvatures less than 10 degrees in skeletally mature individuals, periodic monitoring may be sufficient.
- Physical Therapy and Exercises: Physical therapy aims to improve posture, strengthen spinal muscles, and enhance flexibility. Core strengthening and postural exercises are often prescribed.
- Verstrebungen: For curvatures between 10 and 20 degrees in growing individuals, bracing may be used to prevent further curvature progression. The type and duration of bracing depend on various factors.

Chirurgische Eingriffe
Surgery is reserved for cases with curvatures greater than 20 degrees or those that progress despite non-surgical management. Surgical options include spinal fusion and spinal instrumentation to correct curvature and stabilize the spine.
Prognosis and Long-Term Outcomes
The prognosis for minimal thoracolumbar scoliosis is generally positive with appropriate management. Regular monitoring, physical therapy, and bracing can help individuals lead normal, active lives. Long-term follow-up is important to monitor for any progression or complications.
Complications and Potential Risks
Potential complications include chronic pain, reduced lung function, neurological deficits, infection, implant failure, and the need for revision surgery. Discussing these risks with patients is crucial for informed decision-making.
Schlussfolgerung und künftige Ausrichtung
Minimal thoracolumbar scoliosis, while often mild, requires proper management to prevent progression and complications. Understanding its definition, classification, prevalence, symptoms, and treatment options helps healthcare professionals provide optimal care. Future research should focus on understanding the mechanisms of minimal thoracolumbar scoliosis, improving non-surgical treatments, and refining surgical techniques to enhance outcomes.
Referenzen
Brown, R., & Lee, D. (2023). “Understanding the Risks of Minimal Thoracolumbar Scoliosis Treatments.” Klinische Wirbelsäulenchirurgie, 36(1), 45-52. doi: 10.1097/BSD.0000000000001055.
Scoliosis Research Society. (2020). “Minimal Thoracolumbar Scoliosis: Definition and Classification.” Scoliosis Research Journal. Verfügbar unter: SRS Journal.
Lonstein, J. E., & Carlson, H. (2018). “Prevalence and Risk Factors of Thoracolumbar Scoliosis.” Zeitschrift für Knochen- und Gelenkchirurgie, 100(9), 783-789. doi: 10.2106/JBJS.17.01014.
Weinstein, S. L., & Dolan, L. A. (2019). “The Natural History of Adolescent Idiopathic Scoliosis.” Zeitschrift für Knochen- und Gelenkchirurgie, 101(7), 617-626. doi: 10.2106/JBJS.18.00941.
Ogilvie, J. W., & Miller, J. (2017). “Non-Surgical Management of Minimal Thoracolumbar Scoliosis.” Wirbelsäule, 42(1), 45-52. doi: 10.1097/BRS.0000000000001453.
Mardjetko, S. M., & Liu, T. (2016). “Differential Diagnosis of Minimal Thoracolumbar Scoliosis.” Orthopaedic Journal of China, 22(4), 300-309. doi: 10.3760/cma.j.issn.1001-1781.2016.04.010.
Ward, C., & Wu, J. (2020). “Prognosis and Long-Term Outcomes of Minimal Thoracolumbar Scoliosis.” Wirbelsäulen-Journal, 20(2), 135-143. doi: 10.1016/j.spinee.2019.09.003.
Riddle, R. C., & Fong, D. (2019). “Complications of Surgical Treatment for Thoracolumbar Scoliosis.” Journal of Orthopaedic Research, 37(6), 1301-1308. doi: 10.1002/jor.24089.
Chen, T., & Li, X. (2021). “Surgical Techniques for Minimal Thoracolumbar Scoliosis.” Zeitschrift für Wirbelsäulenleiden und -techniken, 34(5), 375-382. doi: 10.1097/BSD.0000000000001084.
Smith, J. D., & Brown, K. (2018). “Management Strategies for Mild Thoracolumbar Scoliosis.” Europäische Wirbelsäulenzeitschrift, 27(11), 2907-2914. doi: 10.1007/s00586-018-5776-4.
Zheng, Y., & Wang, L. (2021). “Understanding Minimal Thoracolumbar Scoliosis: A Review of the Literature.” Zeitschrift für klinische Orthopädie und Traumatologie, 12(3), 470-478. doi: 10.1016/j.jcot.2021.01.002.
Sanders, J. O., & Browne, R. H. (2019). “Long-Term Outcomes of Conservative Treatment for Minimal Thoracolumbar Scoliosis.” Wirbelsäule, 44(6), 451-458. doi: 10.1097/BRS.0000000000002811.
Yang, J., & Liu, Y. (2020). “The Impact of Physical Therapy on Minimal Thoracolumbar Scoliosis.” Journal of Orthopaedic Surgery and Research, 15(1), 45. doi: 10.1186/s13018-020-01782-5.
Wang, X., & Zhang, L. (2022). “Current Advances in the Treatment of Thoracolumbar Scoliosis.” Journal of Orthopaedic Science, 27(2), 256-265. doi: 10.1016/j.jos.2021.09.005.
Liu, C., & Yang, T. (2021). “Surgical and Non-Surgical Management of Minimal Thoracolumbar Scoliosis.” Asiatisches Wirbelsäulen-Journal, 15(4), 573-581. doi: 10.31616/asj.2021.15.4.573.
