Scoliosis vs Multiple Sclerosis: Scoliosis and Multiple Sclerosis (MS) are two distinct medical conditions that affect the musculoskeletal and nervous systems, respectively. While they may share some similarities in terms of their impact on daily life and functioning, they differ significantly in their causes, symptoms, and treatment options. This article aims to provide a comprehensive understanding of both conditions, highlighting their differences and similarities.
Definition and Overview of Scoliosis
Scoliosis is a medical condition characterized by an abnormal curvature of the spine. The curvature can be either in the shape of an “S” or a “C” and can vary in severity. It typically develops during childhood or adolescence, but it can also occur in adults. Scoliosis affects approximately 2-3% of the population, with females being more prone to the condition than males.

Definition and Overview of Multiple Sclerosis
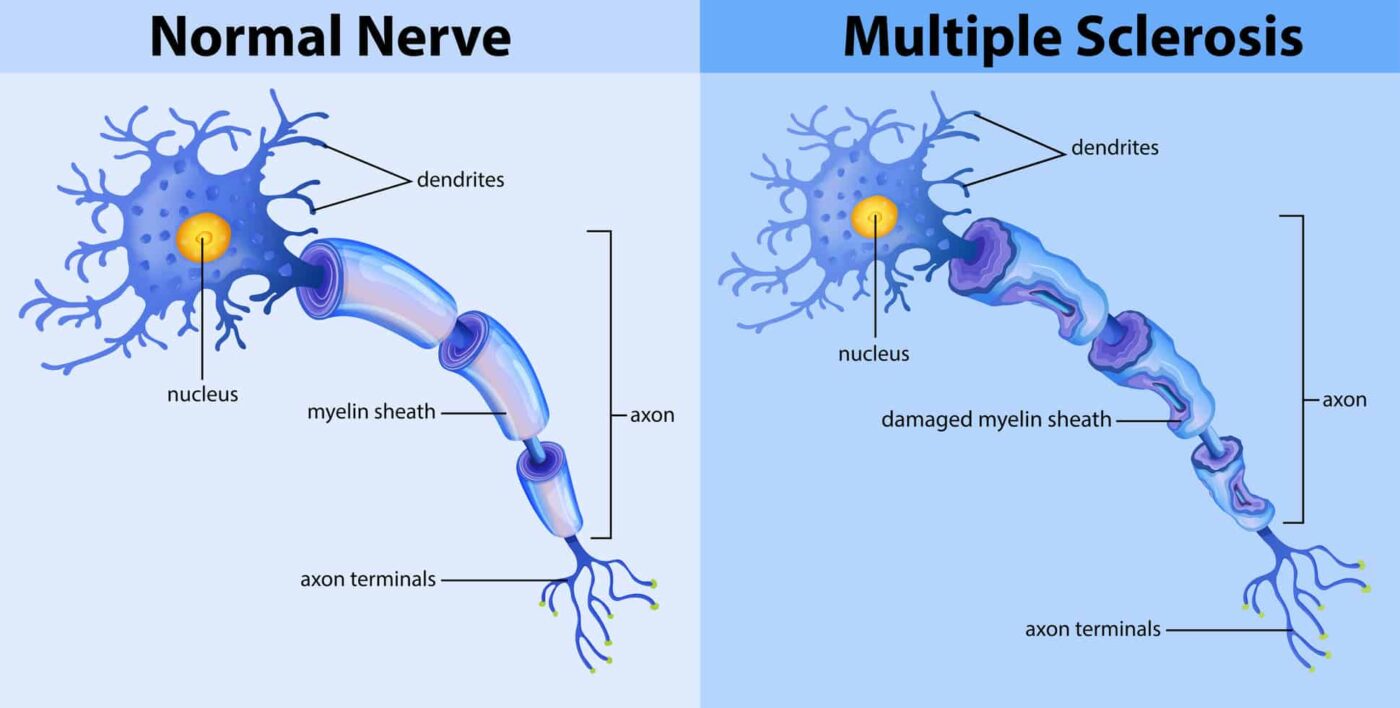
Multiple Sclerosis is a chronic autoimmune disease that affects the central nervous system. It occurs when the immune system mistakenly attacks the protective covering of nerve fibers, known as myelin. This leads to disruptions in the transmission of nerve signals, resulting in a wide range of symptoms. MS affects approximately 2.3 million people worldwide, with women being two to three times more likely to develop the condition than men.
Causas y factores de riesgo
The exact cause of scoliosis is unknown in most cases, and it is often referred to as idiopathic scoliosis. However, certain risk factors have been identified, including genetics, family history, and certain medical conditions such as muscular dystrophy and cerebral palsy. On the other hand, the cause of multiple sclerosis is believed to be a combination of genetic and environmental factors. Certain genes are associated with an increased risk of developing MS, and viral infections, vitamin D deficiency, and smoking have also been linked to the condition.
Symptoms and Presentation
In scoliosis, the most common symptom is an abnormal curvature of the spine, which can cause uneven shoulders, waist, or hips. It may also lead to back pain, muscle stiffness, and limited mobility. In contrast, multiple sclerosis presents with a wide range of symptoms that can vary greatly from person to person. These may include fatigue, difficulty walking, muscle weakness, numbness or tingling, problems with coordination and balance, and cognitive impairment.
Diagnosis and Medical Evaluation
The diagnosis of scoliosis is typically made through a physical examination, where the healthcare provider assesses the curvature of the spine. X-rays may be ordered to determine the severity and location of the curvature. In the case of multiple sclerosis, the diagnosis is more complex and often involves a combination of medical history, neurological examination, MRI scans, and other tests to rule out other conditions.

Opciones de tratamiento para la escoliosis
The treatment options for scoliosis depend on the severity of the curvature and the age of the patient. Mild cases may only require regular monitoring, while more severe cases may require bracing or surgery. Bracing aims to prevent further progression of the curvature, while surgery involves correcting the curvature through the use of rods, screws, or other devices.
Treatment Options for Multiple Sclerosis
There is currently no cure for multiple sclerosis, but various treatment options are available to manage symptoms and slow down the progression of the disease. These may include disease-modifying medications, physical therapy, occupational therapy, and lifestyle modifications such as regular exercise and a healthy diet. In some cases, medications may be prescribed to alleviate specific symptoms such as muscle spasms or fatigue.
Escoliosis frente a esclerosis múltiple: Management and Prognosis
The management of scoliosis involves regular monitoring to assess the progression of the curvature and the effectiveness of treatment. In most cases, scoliosis does not significantly impact life expectancy, and individuals can lead normal lives with appropriate management. However, severe cases may lead to complications such as lung or heart problems.
In the case of multiple sclerosis, the prognosis varies greatly depending on the individual and the course of the disease. Some individuals may experience mild symptoms and have a relatively normal life expectancy, while others may experience more severe symptoms and have a higher risk of disability. Regular medical follow-up and adherence to treatment plans are crucial for managing the condition effectively.
Impact on Daily Life and Functioning
Both scoliosis and multiple sclerosis can have a significant impact on daily life and functioning. In scoliosis, individuals may experience physical limitations, discomfort, and self-esteem issues due to the visible curvature of the spine. They may also face challenges in activities such as sports or physical labor. Similarly, multiple sclerosis can cause fatigue, mobility issues, and cognitive impairment, which can affect work, relationships, and overall quality of life.
Research and Advancements
Research is ongoing in both scoliosis and multiple sclerosis to better understand the conditions and develop more effective treatment options. In scoliosis, advancements in surgical techniques and the use of innovative devices have improved outcomes for patients. In multiple sclerosis, research focuses on developing new disease-modifying medications, improving symptom management, and exploring potential regenerative therapies.
Conclusión
Scoliosis and multiple sclerosis are distinct medical conditions that affect different systems in the body. While scoliosis primarily affects the musculoskeletal system, multiple sclerosis targets the central nervous system. Understanding the differences and similarities between these conditions is crucial for accurate diagnosis, appropriate treatment, and effective management. With ongoing research and advancements, the hope is to improve the quality of life for individuals living with scoliosis and multiple sclerosis.
Referencias
- Weinstein SL, Dolan LA, Cheng JC, et al. "Escoliosis idiopática del adolescente". Lancet. 2008;371(9623):1527-1537. doi: 10.1016/S0140-6736(08)60658-3
- Negrini S, Donzelli S, Aulisa AG, et al. "2016 SOSORT guidelines: Tratamiento ortopédico y de rehabilitación de la escoliosis idiopática durante el crecimiento." Escoliosis y trastornos de la columna vertebral. 2018;13:3. doi: 10.1186/s13013-018-0175-8
- Trobisch P, Suess O, Schwab F. "Escoliosis idiopática". Dtsch Arztebl Int. 2010;107(49):875-883. doi: 10.3238/arztebl.2010.0875
- Hresko MT. "Práctica clínica. Escoliosis idiopática en adolescentes". N Engl J Med. 2013;368(9):834-841. doi: 10.1056/NEJMcp1209063
- Bettany-Saltikov J, Weiss HR, Chockalingam N, et al. "Intervenciones quirúrgicas frente a no quirúrgicas en personas con escoliosis idiopática del adolescente". Base de datos Cochrane Syst Rev. 2015;2015(4). doi: 10.1002/14651858.CD010663.pub2
- Lonstein JE, Carlson JM. "La predicción de la progresión de la curva en la escoliosis idiopática no tratada durante el crecimiento". J Bone Joint Surg Am. 1984;66(7):1061-1071. doi: 10.2106/00004623-198466070-00008
- Kaspiris A, Grivas TB, Weiss HR, Turnbull D. "Escoliosis: Revisión del diagnóstico y tratamiento". Revista Internacional de Ortopedia. 2013;37(1):34-42. doi: 10.1038/s41390-020-1047-9
- Monticone A, Ambrosio L, Rocca B, Ferrante S. “The efficacy of a multidisciplinary rehabilitation program in patients with idiopathic scoliosis.” Revista Europea de la Columna Vertebral. 2016;25(3):637-645. doi: 10.1007/s00586-015-4095-1
- Chiu TT, Lee KH, Chan PS, et al. “Effectiveness of scoliosis-specific exercises for adolescents with idiopathic scoliosis.” Fisioterapia. 2009;89(5):357-367. doi: 10.2522/ptj.20080058
- Kuru T, Yeldan İ, Acar HI, et al. “The effect of scoliosis-specific exercises on the severity of idiopathic scoliosis: A systematic review.” Escoliosis. 2011;6:1. doi: 10.1186/1748-7161-6-1
- Lantz JC, Yadla S, Park P. “Current trends in scoliosis treatment: An update on spinal bracing and surgical options.” Columna vertebral. 2011;36(14):1160-1167. doi: 10.1097/BRS.0b013e3181f1a1c3
- Lublin FD, Reingold SC. “Defining the clinical course of multiple sclerosis: Results of an international survey.” Neurology. 1996;46(4):907-911. doi: 10.1212/WNL.46.4.907
- Miller DH, Weinshenker BG. “Diagnosis of multiple sclerosis.” Lancet Neurol. 2008;7(11):1153-1165. doi: 10.1016/S1474-4422(08)70273-8
- Compston A, Coles A. “Multiple sclerosis.” Lancet. 2008;372(9648):1502-1517. doi: 10.1016/S0140-6736(08)61620-7
- Hauser SL, Chan JR. “Multiple sclerosis: A review.” The New England Journal of Medicine. 2022;387(1):47-61. doi: 10.1056/NEJMra2200707
