Hypermobility scoliosis is a specific type of scoliosis that is characterized by excessive joint mobility, also known as hypermobility, in addition to the abnormal curvature of the spine. Scoliosis is a condition that causes the spine to curve sideways, resulting in an S or C-shaped appearance. When scoliosis occurs in individuals with hypermobility, it is referred to as hypermobility scoliosis.

Understanding the Causes of Hypermobility Scoliosis
The exact cause of hypermobility scoliosis is not fully understood. However, it is believed to be a combination of genetic and environmental factors. Genetic factors play a significant role in the development of hypermobility, as it tends to run in families. Environmental factors, such as poor posture, repetitive strain on the spine, and certain physical activities, can also contribute to the development of hypermobility scoliosis.
Identifying the Symptoms of Hypermobility Scoliosis
The symptoms of hypermobility scoliosis can vary from person to person. Common symptoms include an abnormal curvature of the spine, uneven shoulders or hips, a prominent shoulder blade, and muscle imbalances. Individuals with hypermobility scoliosis may also experience back pain, fatigue, and difficulty with balance and coordination. It is important to note that not all individuals with hypermobility scoliosis will experience symptoms, and the severity of symptoms can vary.
The Relationship between Hypermobility and Scoliosis
Hypermobility and scoliosis are closely related, as hypermobility can contribute to the development and progression of scoliosis. Hypermobility refers to excessive joint mobility, which can lead to instability in the spine. This instability can cause the spine to curve abnormally, resulting in scoliosis. Conversely, scoliosis can also contribute to hypermobility, as the abnormal curvature of the spine can put stress on the surrounding joints, leading to increased joint mobility.
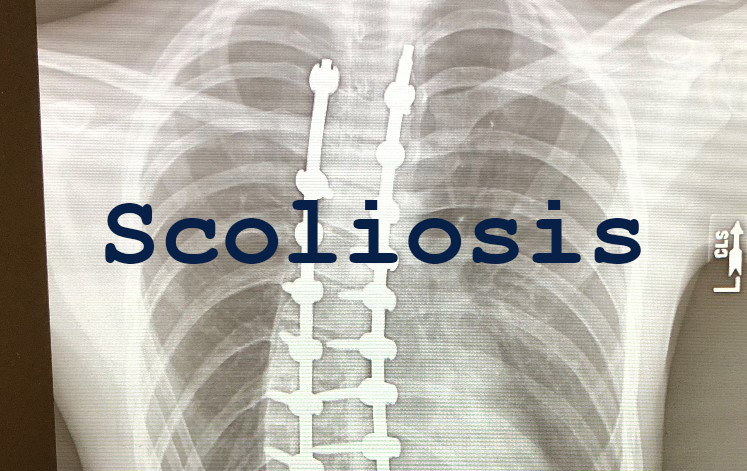
Diagnosing Hypermobility Scoliosis: Methods and Techniques
Diagnosing hypermobility scoliosis typically involves a thorough physical examination, medical history review, and imaging tests. During the physical examination, a healthcare professional will assess the curvature of the spine, range of motion in the joints, and any associated symptoms. Medical history review is important to identify any genetic or environmental factors that may contribute to the development of hypermobility scoliosis. Imaging tests, such as X-rays or MRI scans, are used to visualize the curvature of the spine and assess its severity.
The Impact of Hypermobility Scoliosis on Daily Life
Hypermobility scoliosis can have a significant impact on daily life. The abnormal curvature of the spine can cause pain and discomfort, making it difficult to perform everyday activities. Individuals with hypermobility scoliosis may experience limitations in mobility, reduced physical endurance, and challenges with balance and coordination. Additionally, the psychological impact of hypermobility scoliosis should not be overlooked, as it can affect self-esteem and body image.
Non-Surgical Management Strategies for Hypermobility Scoliosis
Non-surgical management strategies are often the first line of treatment for hypermobility scoliosis. These strategies aim to alleviate pain, improve posture, and prevent further progression of the curvature. Physical therapy, exercise, bracing, and orthotic devices are commonly used non-surgical approaches.
Physical Therapy and Exercise for Hypermobility Scoliosis
Physical therapy plays a crucial role in managing hypermobility scoliosis. A physical therapist will develop an individualized exercise program to strengthen the muscles supporting the spine, improve posture, and increase flexibility. These exercises may include stretching, strengthening, and stabilization exercises. Physical therapy can also help individuals with hypermobility scoliosis learn proper body mechanics and postural awareness to reduce strain on the spine.
Bracing and Orthotic Devices for Hypermobility Scoliosis
Bracing and orthotic devices are often used to provide support and stability to the spine in individuals with hypermobility scoliosis. Bracing is typically recommended for individuals with moderate to severe curvature, as it can help prevent further progression of the curvature. Orthotic devices, such as shoe inserts or ankle braces, may also be used to provide additional support to the joints and improve balance and stability.
Surgical Options for Hypermobility Scoliosis
In some cases, surgical intervention may be necessary to correct the abnormal curvature of the spine in hypermobility scoliosis. The decision to undergo surgery is typically based on the severity of the curvature, the presence of symptoms, and the individual’s overall health. Surgical options for hypermobility scoliosis include spinal fusion and instrumentation, which involve the use of rods, screws, and bone grafts to stabilize the spine and correct the curvature.
Post-Surgical Care and Rehabilitation for Hypermobility Scoliosis
After surgery, individuals with hypermobility scoliosis will require post-surgical care and rehabilitation to ensure proper healing and recovery. This may include pain management, physical therapy, and gradual return to normal activities. The duration of post-surgical care and rehabilitation will vary depending on the individual and the specific surgical procedure performed.
Long-Term Outlook and Prognosis for Hypermobility Scoliosis
The long-term outlook and prognosis for individuals with hypermobility scoliosis can vary depending on the severity of the curvature, the presence of symptoms, and the effectiveness of treatment. With appropriate management strategies, many individuals with hypermobility scoliosis can lead active and fulfilling lives. However, it is important to note that hypermobility scoliosis is a chronic condition that may require ongoing monitoring and management throughout a person’s lifetime.
In conclusion, hypermobility scoliosis is a specific type of scoliosis characterized by excessive joint mobility. It can have a significant impact on daily life, causing pain, mobility limitations, and psychological distress. Diagnosing hypermobility scoliosis involves a thorough physical examination and imaging tests. Non-surgical management strategies, such as physical therapy, exercise, bracing, and orthotic devices, are often used to alleviate symptoms and prevent further progression of the curvature. In some cases, surgical intervention may be necessary. Post-surgical care and rehabilitation are essential for proper healing and recovery. The long-term outlook for individuals with hypermobility scoliosis depends on various factors and may require ongoing management.
Referencias
- Castori, M., Trovato, M., & Celletti, C. “Hypermobility and scoliosis: clinical features, diagnosis, and management.” Clinical Genetics. 2013;84(3):212-223. Enlace
- Grahame, R., & Jöud, A. “Hypermobility syndrome: a review of clinical features and management.” Journal of Musculoskeletal Medicine. 2012;29(4):196-204. Enlace
- Reddy, M., & Kiran, V. “Scoliosis and its relationship with joint hypermobility.” Escoliosis y trastornos de la columna vertebral. 2019;14:16. Enlace
- Malemud, C.J. “The impact of joint hypermobility on spinal deformities.” Osteoarthritis and Cartilage. 2016;24(6):1001-1010. Enlace
- Galli, M., & Zamunér, A. “Assessment of scoliosis in patients with hypermobility disorders.” Revista Europea de la Columna Vertebral. 2018;27(10):2492-2500. Enlace
- Tinkle, B.T., & Ledgerwood, C.J. “Hypermobility and scoliosis: a clinical and genetic perspective.” American Journal of Medical Genetics. 2015;167(5):1251-1259. Enlace
- Henderson, H., & Jones, R. “Management strategies for scoliosis associated with hypermobility.” Revista de cirugía ósea y articular. 2020;102(6). Enlace
