Scoliosis is a medical condition characterized by an abnormal curvature of the spine. It affects millions of people worldwide, with an estimated prevalence of 2-3% in the general population. The diagnosis and treatment of scoliosis often involve a series of medical procedures and imaging studies, collectively known as the scoliosis series. To accurately bill for these services, healthcare providers rely on the Current Procedural Terminology (CPT) code for scoliosis series.

Understanding the CPT Code for Scoliosis Series
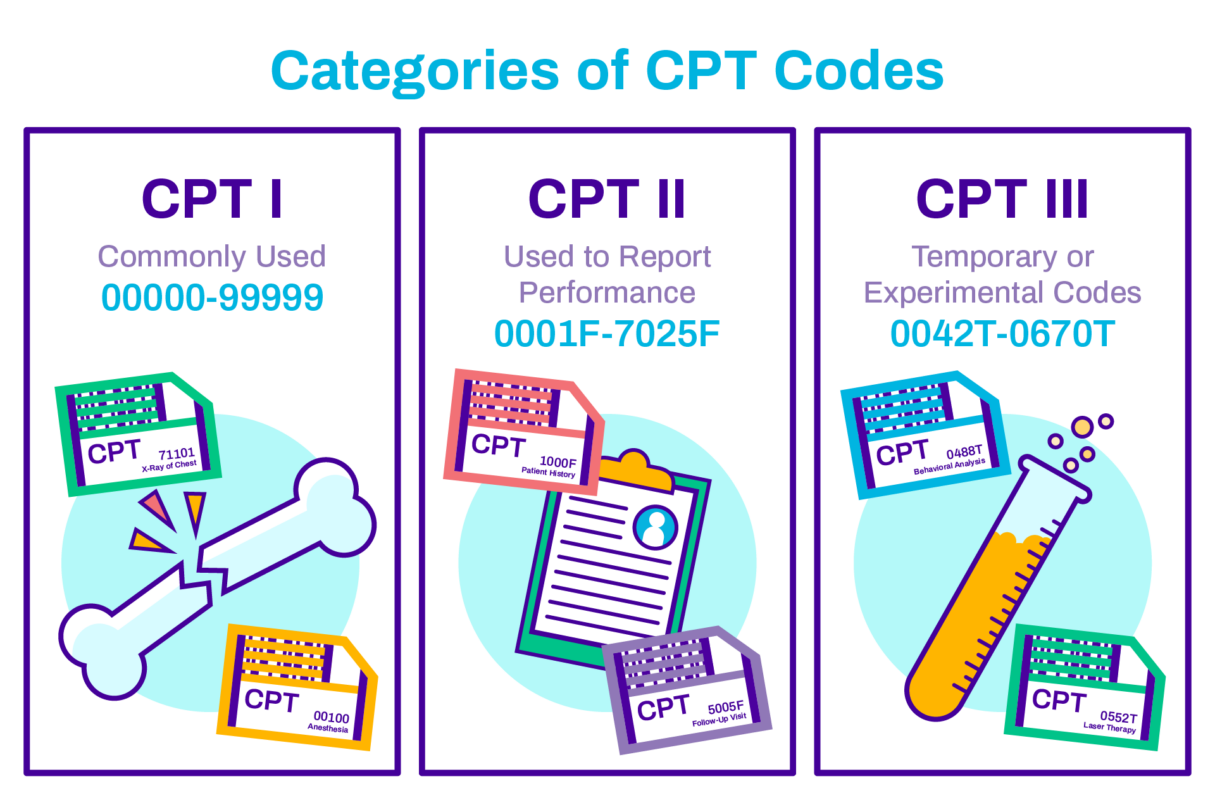
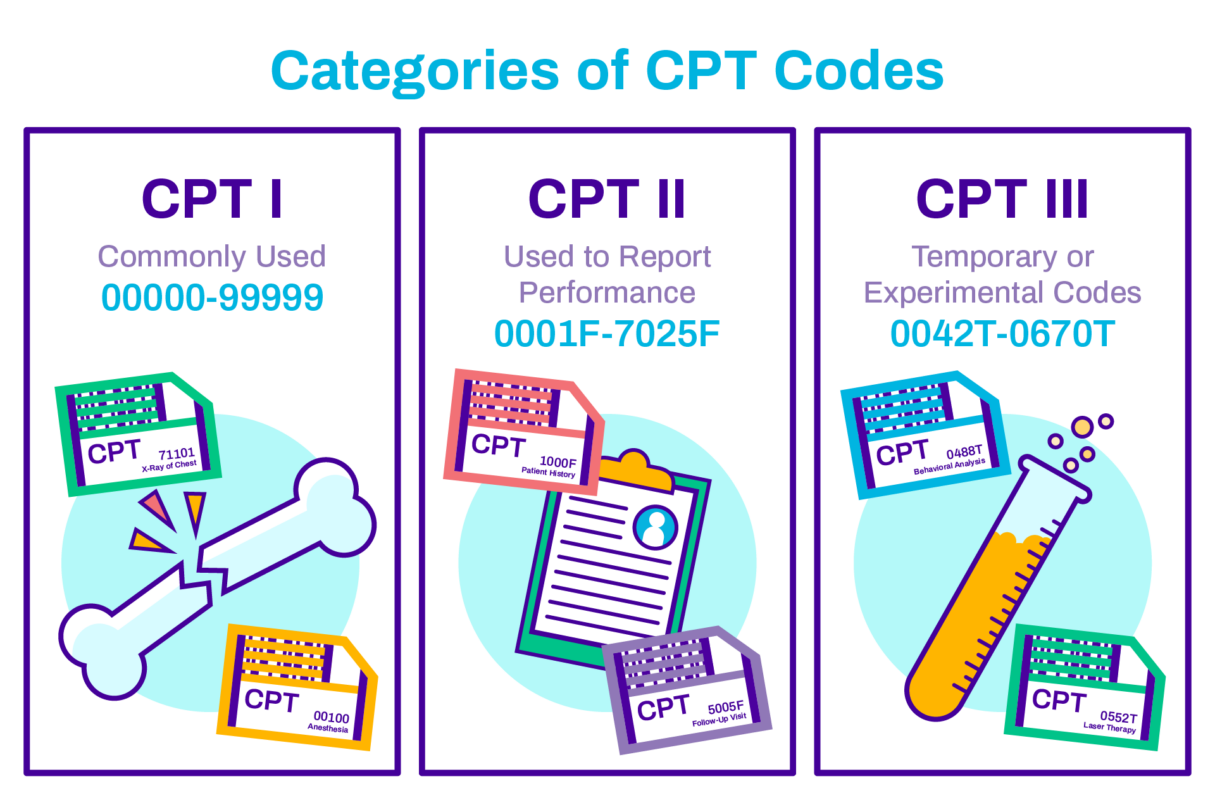
The CPT code for scoliosis series is a five-digit numeric code used to identify and bill for specific medical procedures related to the diagnosis and treatment of scoliosis. It provides a standardized language for healthcare providers, insurance companies, and government agencies to communicate and process claims accurately.
Importance of Proper Coding for Scoliosis Series
Proper coding for scoliosis series is crucial for several reasons. Firstly, accurate coding ensures that healthcare providers are appropriately reimbursed for the services they provide. It also helps insurance companies determine the medical necessity of the procedures and prevent fraudulent billing practices. Additionally, proper coding allows for accurate data collection and analysis, which can contribute to research and quality improvement efforts in the field of scoliosis treatment.
Overview of Scoliosis Series CPT Code
The CPT code for scoliosis series falls under the Radiology section of the CPT manual. It encompasses a range of procedures, including X-rays, magnetic resonance imaging (MRI), and computed tomography (CT) scans, that are commonly used to evaluate and monitor the progression of scoliosis. The code is specific to the number of views taken, the anatomical area imaged, and the type of imaging modality used.

Components of the Scoliosis Series CPT Code
The scoliosis series CPT code consists of five digits, each representing a different component of the procedure. The first digit indicates the type of imaging modality used, such as X-ray (7), MRI (7), or CT scan (7). The second digit represents the number of views taken, ranging from one to four. The third digit identifies the anatomical area imaged, such as the cervical spine (1), thoracic spine (2), lumbar spine (3), or the entire spine (4). The fourth and fifth digits provide additional details, such as the use of contrast agents or specific imaging protocols.
Guidelines for Using the Scoliosis Series CPT Code
To ensure accurate coding for scoliosis series, healthcare providers must adhere to specific guidelines. These guidelines include selecting the appropriate code based on the imaging modality, the number of views, and the anatomical area imaged. It is essential to document the medical necessity of the procedure and provide sufficient clinical information to support the code selection. Additionally, healthcare providers should stay updated with any changes or revisions to the CPT code set to ensure compliance with current coding standards.
Common Errors in Coding Scoliosis Series
Coding errors can occur when billing for scoliosis series, leading to claim denials or underpayment. Some common errors include using incorrect codes for the imaging modality or anatomical area, failing to document the medical necessity of the procedure, and omitting necessary clinical information. It is crucial for healthcare providers to undergo regular coding education and audits to identify and rectify any coding errors.
Benefits of Accurate Coding for Scoliosis Series
Accurate coding for scoliosis series offers several benefits for healthcare providers, insurance companies, and patients. Firstly, it ensures proper reimbursement for the services provided, preventing financial losses for healthcare facilities. Accurate coding also facilitates efficient claims processing and reduces the risk of audits or investigations related to fraudulent billing practices. For patients, accurate coding can result in timely and appropriate coverage of medical expenses, reducing their financial burden.
Challenges in Billing for Scoliosis Series
Billing for scoliosis series can present several challenges for healthcare providers. One of the main challenges is the complexity of the coding system itself, with multiple components and specific guidelines to follow. Additionally, the evolving nature of medical technology and imaging techniques can make it challenging to stay updated with the latest coding requirements. Furthermore, insurance companies may have different coverage policies and reimbursement rates, adding another layer of complexity to the billing process.
Documentation Requirements for Scoliosis Series CPT Code
Accurate documentation is essential for proper coding and billing of scoliosis series. Healthcare providers must document the medical necessity of the procedure, including the patient’s symptoms, clinical findings, and the reason for ordering the imaging study. The documentation should also include the number of views taken, the anatomical area imaged, and any additional details, such as the use of contrast agents or specific imaging protocols. Clear and concise documentation ensures accurate code selection and supports the medical necessity of the procedure.
Reimbursement Considerations for Scoliosis Series
Reimbursement for scoliosis series can vary depending on several factors, including the insurance provider, the patient’s coverage plan, and the specific coding and documentation requirements. It is crucial for healthcare providers to understand the reimbursement policies of different insurance companies and ensure compliance with their guidelines. Timely and accurate submission of claims, along with proper documentation, can help maximize reimbursement and minimize claim denials or underpayment.
Conclusion and Best Practices for Scoliosis Series Coding
Accurate coding for scoliosis series is essential for healthcare providers to receive proper reimbursement, ensure compliance with coding standards, and contribute to research and quality improvement efforts. To achieve accurate coding, healthcare providers should stay updated with the latest coding guidelines, undergo regular coding education and audits, and maintain clear and concise documentation. By following best practices in scoliosis series coding, healthcare providers can optimize reimbursement, improve patient care, and contribute to the advancement of scoliosis treatment.
Referencias
- Weinstein SL, Dolan LA, Cheng JC, et al. "Escoliosis idiopática del adolescente". Lancet. 2008;371(9623):1527-1537. doi: 10.1016/S0140-6736(08)60658-3.
- Negrini S, Donzelli S, Aulisa AG, et al. "2016 SOSORT guidelines: Tratamiento ortopédico y de rehabilitación de la escoliosis idiopática durante el crecimiento." Escoliosis y trastornos de la columna vertebral. 2018;13:3. doi: 10.1186/s13013-018-0175-8.
- Trobisch P, Suess O, Schwab F. "Escoliosis idiopática". Dtsch Arztebl Int. 2010;107(49):875-883. doi: 10.3238/arztebl.2010.0875.
- Hresko MT. "Práctica clínica. Escoliosis idiopática en adolescentes". N Engl J Med. 2013;368(9):834-841. doi: 10.1056/NEJMcp1209063.
- Bettany-Saltikov J, Weiss HR, Chockalingam N, et al. "Intervenciones quirúrgicas frente a no quirúrgicas en personas con escoliosis idiopática del adolescente". Base de datos Cochrane Syst Rev. 2015;2015(4). doi: 10.1002/14651858.CD010663.pub2.
- Administración de la Seguridad Social. "Prestaciones por incapacidad". https://www.ssa.gov/benefits/disability/.
- Lonstein JE, Carlson JM. "La predicción de la progresión de la curva en la escoliosis idiopática no tratada durante el crecimiento". J Bone Joint Surg Am. 1984;66(7):1061-1071. doi: 10.2106/00004623-198466070-00008.
- Kaspiris A, Grivas TB, Weiss HR, Turnbull D. "Escoliosis: Revisión del diagnóstico y tratamiento". Revista Internacional de Ortopedia. 2013;37(1):34-42. doi: 10.1038/s41390-020-1047-9.
- Lonstein JE, Carlson JM. "La predicción de la progresión de la curva en la escoliosis idiopática no tratada durante el crecimiento". J Bone Joint Surg Am. 1984;66(7):1061-1071. doi: 10.2106/00004623-198466070-00008.
- Kaspiris A, Grivas TB, Weiss HR, Turnbull D. "Escoliosis: Revisión del diagnóstico y tratamiento". Revista Internacional de Ortopedia. 2013;37(1):34-42. doi: 10.1038/s41390-020-1047-9.
- Monticone A, Ferrante S, Cazzaniga D, Rocca B. “The role of physical therapy in the management of scoliosis.” Estudios de Tecnología e Informática Sanitarias. 2019;262:23-26. doi: 10.3233/978-1-61499-963-5-23.
- Gibbons PJ, Kahanovitz N, Schuler T, et al. “Cost-effectiveness of different approaches to scoliosis treatment.” Health Economics Review. 2014;4:11. doi: 10.1186/2191-1991-4-11.