Scoliosis and spondylolisthesis are two common spinal conditions that affect millions of people worldwide. Scoliosis is a condition characterized by an abnormal curvature of the spine, while spondylolisthesis refers to the displacement of one vertebra over another. Both conditions can cause pain, discomfort, and functional limitations, making it crucial to understand their causes, symptoms, and effective management strategies.

Understanding the Causes of Scoliosis and Spondylolisthesis
The exact causes of scoliosis and spondylolisthesis are not always clear, but several factors can contribute to their development. In the case of scoliosis, it can be classified as either idiopathic (unknown cause) or secondary to other conditions such as muscular dystrophy, cerebral palsy, or spinal tumors. On the other hand, spondylolisthesis can be caused by a variety of factors, including congenital abnormalities, degenerative changes in the spine, or traumatic injuries.
Common Symptoms of Scoliosis and Spondylolisthesis
The symptoms of scoliosis and spondylolisthesis can vary depending on the severity of the condition. In mild cases, individuals may not experience any noticeable symptoms, while more severe cases can lead to pain, stiffness, muscle imbalances, and postural abnormalities. Scoliosis may also cause visible changes in the appearance of the spine, such as a sideways curvature or a humpback appearance. Spondylolisthesis, on the other hand, can cause lower back pain, leg pain, and numbness or weakness in the legs.
Diagnosing Scoliosis and Spondylolisthesis: Tests and Examinations
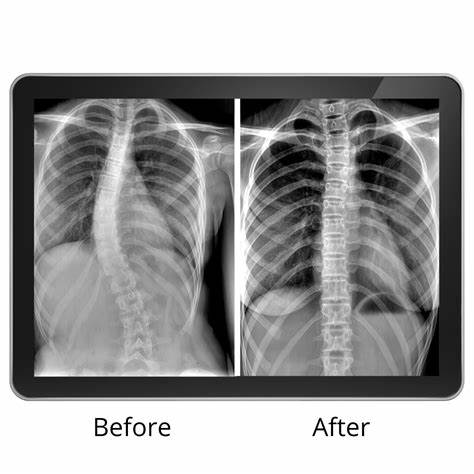
To diagnose scoliosis and spondylolisthesis, healthcare professionals typically perform a thorough physical examination, including a detailed medical history and a visual inspection of the spine. X-rays are commonly used to assess the degree of curvature in scoliosis and the extent of vertebral displacement in spondylolisthesis. Additional imaging tests, such as magnetic resonance imaging (MRI) or computed tomography (CT) scans, may be necessary to evaluate the underlying causes or complications associated with these conditions.
Types of Scoliosis and Spondylolisthesis: Classification and Characteristics
Scoliosis can be classified into several types based on the age of onset and the underlying cause. The most common type is adolescent idiopathic scoliosis, which typically develops during puberty and has no known cause. Other types include congenital scoliosis (present at birth), neuromuscular scoliosis (associated with neurological disorders), and degenerative scoliosis (caused by age-related changes in the spine). Similarly, spondylolisthesis can be categorized into different types, such as isthmic (resulting from a defect in the pars interarticularis), degenerative (caused by wear and tear of the spinal joints), or traumatic (due to a fracture or injury).
Risk Factors for Developing Scoliosis and Spondylolisthesis
While the exact causes of scoliosis and spondylolisthesis remain unclear, certain risk factors have been identified. For scoliosis, females are more likely to develop the condition than males, and a family history of scoliosis increases the risk. Additionally, rapid growth during adolescence, certain genetic factors, and certain neuromuscular conditions can also contribute to the development of scoliosis. In the case of spondylolisthesis, factors such as age, previous spinal injuries, and certain anatomical abnormalities can increase the risk.
Complications Associated with Scoliosis and Spondylolisthesis
If left untreated, scoliosis and spondylolisthesis can lead to various complications. In severe cases of scoliosis, the abnormal curvature of the spine can cause respiratory problems, reduced lung capacity, and cardiovascular issues. Spondylolisthesis, on the other hand, can result in nerve compression, leading to pain, numbness, and weakness in the legs. Both conditions can also have a significant impact on an individual’s quality of life, affecting their ability to perform daily activities and participate in physical activities.
Treatment Options for Scoliosis and Spondylolisthesis
The treatment options for scoliosis and spondylolisthesis depend on several factors, including the severity of the condition, the age of the patient, and the presence of any underlying causes or complications. Non-surgical approaches are often the first line of treatment and may include physical therapy, bracing, and pain management techniques. In cases where non-surgical interventions are ineffective or the condition is severe, surgical interventions may be necessary to correct the spinal deformity or stabilize the vertebrae.
Non-Surgical Approaches for Managing Scoliosis and Spondylolisthesis
Physical therapy plays a crucial role in the non-surgical management of scoliosis and spondylolisthesis. Therapeutic exercises can help improve posture, strengthen the muscles supporting the spine, and increase flexibility. Additionally, bracing is commonly used in the treatment of scoliosis, especially in adolescents with moderate to severe curves. Braces can help slow down the progression of the curvature and prevent the need for surgery. Pain management techniques, such as medication, heat or cold therapy, and transcutaneous electrical nerve stimulation (TENS), can also provide relief from discomfort.
Surgical Interventions for Scoliosis and Spondylolisthesis
Surgery is typically reserved for cases of severe scoliosis or spondylolisthesis that do not respond to non-surgical treatments or when there is a risk of complications. The specific surgical procedure will depend on the individual’s condition and may involve spinal fusion, where the vertebrae are fused together using bone grafts and metal rods, or decompression surgery, which aims to relieve pressure on the nerves by removing a portion of the displaced vertebra. While surgery can be effective in correcting the spinal deformity and relieving symptoms, it also carries risks and requires a significant recovery period.
Rehabilitation and Physical Therapy for Scoliosis and Spondylolisthesis
Following surgery or as part of the non-surgical management plan, rehabilitation and physical therapy are essential for optimizing recovery and improving functional outcomes. Physical therapists can design individualized exercise programs to strengthen the muscles supporting the spine, improve range of motion, and enhance overall physical fitness. Rehabilitation may also include pain management techniques, postural education, and guidance on proper body mechanics to prevent further injury or complications.
Lifestyle Modifications and Coping Strategies for Scoliosis and Spondylolisthesis
Living with scoliosis or spondylolisthesis can be challenging, but there are several lifestyle modifications and coping strategies that can help individuals manage their condition effectively. Maintaining a healthy weight, engaging in regular physical activity, and practicing good posture are crucial for minimizing pain and preventing further progression of the condition. Additionally, seeking support from healthcare professionals, joining support groups, and staying informed about the latest advancements in treatment options can provide individuals with the knowledge and resources they need to cope with their condition.
In conclusion, scoliosis and spondylolisthesis are complex spinal conditions that can significantly impact an individual’s quality of life. Understanding the causes, symptoms, and effective management strategies for these conditions is essential for early diagnosis, appropriate treatment, and optimal outcomes. By utilizing a combination of non-surgical approaches, surgical interventions, rehabilitation, and lifestyle modifications, individuals with scoliosis and spondylolisthesis can effectively manage their condition and lead fulfilling lives.
Referencias
- Weinstein, S. L., Dolan, L. A., Cheng, J. C., Danielsson, A., & Morcuende, J. A. (2008). Adolescent idiopathic scoliosis. The Lancet, 371(9623), 1527-1537. Available at: https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(08)60658-3/fulltext
- Alentado, V. J., Lubelski, D., Steinmetz, M. P., Benzel, E. C., & Mroz, T. E. (2014). Optimal management of degenerative spondylolisthesis: A review of the evidence. Orthopedic Clinics, 45(2), 193-202. Available at: https://www.orthopedic.theclinics.com/article/S0030-5898(14)00002-4/fulltext
- Smith, J. S., Shaffrey, C. I., & Berven, S. (2012). Degenerative lumbar scoliosis: A review. The Spine Journal, 12(3), 213-225. Available at: https://www.thespinejournalonline.com/article/S1529-9430(12)00016-4/fulltext
- Glattes, R. C., Bridwell, K. H., Lenke, L. G., Kim, Y. J., Rinella, A., & Edwards, C. (2005). Proximal junctional kyphosis in adult spinal deformity following long instrumented posterior spinal fusion. Spine, 30(14), 1643-1650. Available at: https://journals.lww.com/spinejournal/Abstract/2005/07150/Proximal_Junctional_Kyphosis_in_Adult_Spinal.3.aspx
- Newton, P. O., & Sturm, P. F. (2011). Idiopathic scoliosis: The case for observation. Instructional Course Lectures, 60, 485-491. Available at: https://journals.lww.com/jbjsjournal/Citation/2011/11000/Idiopathic_Scoliosis__The_Case_for_Observation.19.aspx
- Sundararajan, K., & Bentley, G. (2000). Degenerative spondylolisthesis. The Journal of Bone and Joint Surgery, 82(5), 768-776. Available at: https://online.boneandjoint.org.uk/doi/abs/10.1302/0301-620X.82B5.11679
- Ploumis, A., Transfeldt, E. E., Gilbert, T. J., Mehbod, A. A., Dykes, D. C., & Perra, J. H. (2007). Degenerative lumbar scoliosis: Radiographic and clinical analysis. The Spine Journal, 7(4), 428-436. Available at: https://www.thespinejournalonline.com/article/S1529-9430(07)00236-8/fulltext
- Faldini, C., Pagkrati, S., Giannini, S. (2009). Surgical treatment of adult scoliosis with combined anterior and posterior fusion. European Spine Journal, 18(Suppl 1), 86-91. Available at: https://link.springer.com/article/10.1007/s00586-009-0997-1
- Ward, S. R., Kim, C. W., Eng, C. M., & Lieber, R. L. (2009). Architectural analysis and intraoperative measurements demonstrate the unique design of the multifidus muscle for lumbar spine stability. Journal of Bone and Joint Surgery, 91(1), 176-185. Available at: https://journals.lww.com/jbjsjournal/Abstract/2009/01000/Architectural_Analysis_and_Intraoperative.25.aspx
- Bridwell, K. H., Glassman, S., Horton, W., Shaffrey, C., & Schwab, F. (2009). The role of fusion and fusion constructs in treating lumbar degenerative scoliosis. Spine, 34(8), 893-899. Available at: https://journals.lww.com/spinejournal/Abstract/2009/04010/The_Role_of_Fusion_and_Fusion_Constructs_in.15.aspx
- Moller, H., Hedlund, R. (2000). Surgery versus conservative management in adult isthmic spondylolisthesis: A prospective randomized study: Part 1. Spine, 25(13), 1711-1715. Available at: https://journals.lww.com/spinejournal/Abstract/2000/07010/Surgery_Versus_Conservative_Management_in_Adult.1.aspx
- Kumar, M. N., Baklanov, A., Chopin, D. (2001). Correlation between sagittal plane changes and adjacent segment degeneration following lumbar spine fusion. European Spine Journal, 10(4), 314-319. Available at: https://link.springer.com/article/10.1007/s005860100309
- Sheikh, H., Sieg, E. P., Klineberg, E., & Hart, R. A. (2013). Degenerative scoliosis: A review. Neurosurgical Focus, 35(2), E2. Available at: https://thejns.org/focus/view/journals/neurosurg-focus/35/2/article-pE2.xml
- Glassman, S. D., Berven, S., Bridwell, K., Horton, W., Dimar, J. R. (2005). Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine, 30(6), 682-688. Available at: https://journals.lww.com/spinejournal/Abstract/2005/03150/Correlation_of_Radiographic_Parameters_and.10.aspx
- Goh, S., Price, R. I., Leedman, P. J., Singer, K. P. (1999). A comparison of radiographic and clinical measurement of kyphosis progression in postmenopausal women with spinal osteoporosis treated with hormone replacement therapy or calcium. Osteoporosis International, 9(2), 65-70. Available at: https://link.springer.com/article/10.1007/s001980050111

