Scoliosis is a common yet often overlooked spinal issue, particularly during the growth period of adolescence. It can result in bodily asymmetry, affecting posture and quality of life, with severe cases potentially impacting respiratory and cardiac functions.
Definition and Symptoms of Scoliosis:
Scoliosis is a structural disorder affecting the spine, typically characterized by lateral curvature along its vertical axis. This curvature may occur in various parts of the spine, with the thoracic or lumbar regions being most common. While a normal spine axis should be straight, scoliosis can manifest as an “S” or “C” shape. The symptoms vary based on the patient’s age, severity of the condition, and location of the curvature. In adolescence, symptoms often surface during rapid growth, including bodily asymmetry, uneven shoulders, pelvic tilt, and noticeable spinal curvature. These symptoms may lead to feelings of self-consciousness, affecting body image and confidence.
Apart from visible changes, scoliosis can also induce other health issues. Significant spinal curvature may restrict respiratory and cardiac functions due to the impact on thoracic cavity space. Additionally, scoliosis may cause muscle imbalances in the back, leading to chronic back pain.
Not all cases exhibit clear symptoms, especially in the early stages. Thus, early screening and diagnosis become crucial to implementing timely intervention.
Basic Principles of Scoliosis Screening:
Scoliosis screening is a vital measure aimed at early detection and intervention in spinal curvature issues. To ensure the effectiveness and accuracy of screening, certain fundamental principles must be followed.
Careful selection of screening subjects is crucial, primarily focusing on pre-school and adolescent individuals. Regular screening, particularly during growth stages, is recommended. Special attention during school entry and adolescence, along with regular follow-up screenings for those previously diagnosed with scoliosis, is essential.
Involvement of professionals is necessary for accurate and effective scoliosis screening. Physicians, physical therapists, and other medical professionals play crucial roles in the screening process, employing their expertise to identify signs through physical examinations and relevant medical imaging.
Once signs of scoliosis are identified, timely adoption of appropriate treatment and management measures is crucial. This may include regular follow-ups, physical therapy, specialized exercise plans, or, in certain cases, surgery.
Steps of Scoliosis Screening Procedure:
The scoliosis screening procedure involves a systematic and detailed series of steps to early identify individuals at risk of spinal curvature. Key steps include:
Preliminary Assessment and Medical History Collection: Healthcare professionals engage in conversations with individuals and their families to understand the individual’s physical condition, family medical history, and any spinal-related symptoms, helping determine the risk factors for scoliosis.
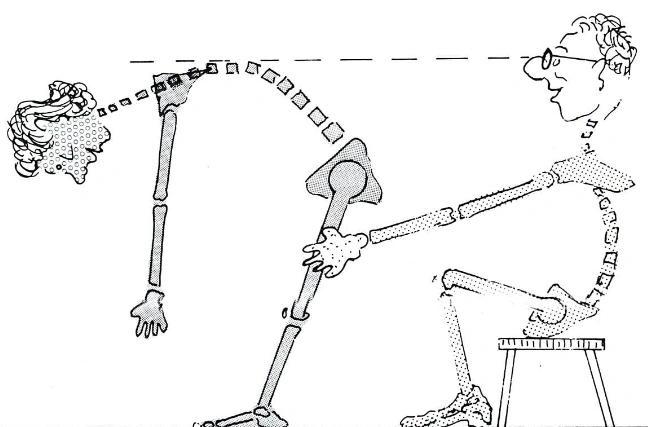
Physical Examination and Posture Assessment: Physicians conduct detailed examinations of the back, shoulders, and pelvis, observing for asymmetry, muscle imbalances, or other anomalies. Careful observation aids in the preliminary assessment of potential scoliosis.
1. The patient begins by standing erect (shoulders back, head up, gaze ahead, arms hanging loosely at their sides, knees straight, and facing away with the their back to the screener).
The screener should check for the following:
· One shoulder higher than the other
· One shoulder blade higher or more prominent than the other
· One hip higher than the other
· Space between arms and body greater on one side
· Waist creases uneven
· Obvious lateral curvature of the spine
· Observe from either left or right side for kyphosis (increased curve of thoracic spine) or lordosis (increased curve in lumbar area)
2. The next position is the Adams Forward Bend Test. With palms together, chin to the chest, the student bends forward until the back is horizontal. Screeners should check for:
· Asymmetry of two sides of the back
· Rib prominence
3. The final portion is using a scoliometer. This is considered best practice and should be used if at all possible. It is similar to a carpenter’s level and designed to measure the degree of spinal rotation.
· Hold the scoliometer with the number “0” directly over the top ridge of the spine
· Do not press down as this will distort the reading
· A reading should be taken at both the thoracic and lumber spine

X-ray Examination and Other Medical Imaging: X-rays provide detailed information about spinal structure, including the degree and location of curvature. This diagnostic imaging is crucial for confirming scoliosis and assessing the severity, forming the basis for subsequent treatment plans.
Comprehensive Assessment by Professional Physicians: Combining medical history, physical examination, and medical imaging results, physicians make a comprehensive judgment on the presence and severity of scoliosis. Based on this assessment, personalized treatment plans, including monitoring, physical therapy, special exercises, or surgery, can be devised.
Introduction to Forethought Versión Profesional Ⅱ:
Forethought Professional Version Ⅱ is an advanced medical imaging processing software designed specifically check for scoliosis screening. Its unique algorithms and cutting-edge image recognition technology allow precise measurement and analysis of spinal curvature, providing healthcare professionals with comprehensive and visual assessment tools.
One notable feature is its high level of automation. Forethought Professional Version Ⅱ efficiently processes large volumes of medical imaging data, reducing the workload on physicians and enhancing screening efficiency. Its intelligent algorithms rapidly identify potential signs of scoliosis, offering physicians a more accurate initial assessment.
Forethought Professional Version Ⅱ also boasts a user-friendly interface and robust data management features. Physicians can easily view and compare patient medical images, monitoring spinal changes in real-time. This real-time monitoring helps physicians better understand the development trends of the condition, facilitating the creation of more personalized treatment plans.
Forethought Professional Version Ⅱ, as a professional scoliosis screening device, enables us to better protect patients’ spinal health and provide them with more comprehensive medical services.
As a continually upgraded and optimized product by Forethought, Forethought Professional Version Ⅱ exhibits high scalability, adapting to diverse medical environments and needs.
Referencias
- [1] Weinstein SL, Dolan LA, Cheng JC, et al. "Escoliosis idiopática adolescente". Lancet. 2008;371(9623):1527-1537. doi: 10.1016/S0140-6736(08)60658-3.
- [2] Negrini S, Donzelli S, Aulisa AG, et al. "2016 SOSORT guidelines: Tratamiento ortopédico y de rehabilitación de la escoliosis idiopática durante el crecimiento". Escoliosis y trastornos de la columna vertebral. 2018;13:3. doi: 10.1186/s13013-018-0175-8.
- [3] Trobisch P, Suess O, Schwab F. "Escoliosis idiopática". Dtsch Arztebl Int. 2010;107(49):875-883. doi: 10.3238/arztebl.2010.0875.
- [4] Hresko MT. "Práctica clínica. Escoliosis idiopática en adolescentes". N Engl J Med. 2013;368(9):834-841. doi: 10.1056/NEJMcp1209063.
- [5] Bettany-Saltikov J, Weiss HR, Chockalingam N, et al. "Intervenciones quirúrgicas versus no quirúrgicas en personas con escoliosis idiopática del adolescente". Cochrane Database Syst Rev. 2015;2015(4). doi: 10.1002/14651858.CD010663.pub2.
- [6] Lonstein JE, Carlson JM. “The prediction of curve progression in untreated idiopathic scoliosis during growth.” J Bone Joint Surg Am. 1984;66(7):1061-1071. doi: 10.2106/00004623-198466070-00008.
- [7] Kaspiris A, Grivas TB, Weiss HR, Turnbull D. “Scoliosis: Review of diagnosis and treatment.” International Journal of Orthopaedics. 2013;37(1):34-42. doi: 10.1038/s41390-020-1047-9.
- [8] Monticone M, Ambrosini E, Cazzaniga D, et al. “Active self-correction and task-oriented exercises reduce spinal deformity and improve quality of life in subjects with mild adolescent idiopathic scoliosis: Results of a randomized controlled trial.” Eur Spine J. 2016;25(10):3118-3127. doi: 10.1007/s00586-016-4625-4.
- [9] Kotwicki T, Negrini S, Grivas TB, et al. “Methodology of evaluation of scoliosis, back deformities and posture.” Scoliosis. 2009;4:26. doi: 10.1186/1748-7161-4-26.
- [10] Sanders JO, Browne RH, McConnell SJ, et al. “Maturity assessment and curve progression in girls with idiopathic scoliosis.” Journal of Bone and Joint Surgery. 2007;89(1):64-73. doi: 10.2106/JBJS.F.00004.
- [11] Negrini S, Hresko TM, O’Brien JP, et al. “Recommendations for research studies on treatment of idiopathic scoliosis: Consensus 2014 between SOSORT and SRS Non-Operative Management Committee.” Scoliosis and Spinal Disorders. 2015;10:8. doi: 10.1186/s13013-015-0032-4.
- [12] Glassman SD, Berven S, Kostuik J, et al. “Scoliosis Research Society Instrument Validation Study: A Multicenter Assessment of Surgical Outcomes in Idiopathic Scoliosis.” Spine. 2005;30(6):699-702. doi: [10.1097/01.brs.0000157447.56975.3e](https://doi.org/10.1097/01.brs