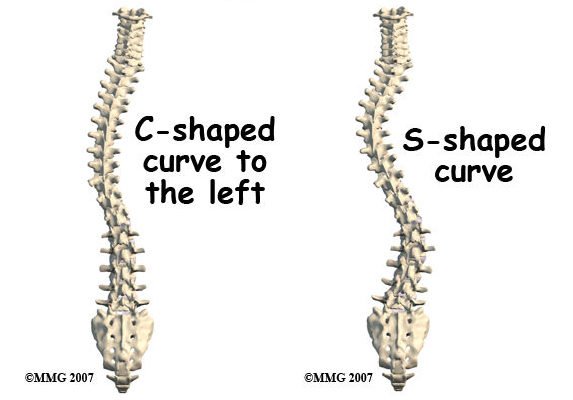
Scoliosis is a medical condition characterized by an abnormal sideways curvature of the spine, forming an “S” or “C” shape. The severity of the curvature can range from mild to severe, affecting different parts of the spine. Scoliosis is classified into structural and nonstructural types. Structural scoliosis results from a physical abnormality in the spine, whereas nonstructural scoliosis is temporary and can be corrected by addressing the underlying cause.
Causes and Risk Factors of Scoliosis
The exact cause of scoliosis is often unknown, though it can develop in otherwise healthy individuals. Risk factors include genetic predisposition, as scoliosis tends to run in families, with a higher prevalence among females. Other contributing factors include medical conditions such as muscular dystrophy and cerebral palsy, as well as previous spine surgeries or injuries.
Types and Classification of Scoliosis Series
Scoliosis is classified based on onset age, cause, and curvature location. Common types include:
- Scoliose idiopathique : No known cause.
- Scoliose congénitale : Present at birth due to abnormal spinal development.
- Scoliose neuromusculaire : Associated with conditions like cerebral palsy.
- Degenerative Scoliosis: Results from age-related changes in the spine.
Signs and Symptoms of Scoliosis
Signs and symptoms vary with the curvature’s severity. Mild scoliosis may present with minimal symptoms, while severe cases might show an uneven waistline, one shoulder higher than the other, or a visible spinal curve. Some individuals may also experience back pain, muscle stiffness, or difficulty breathing if the curvature affects the chest area.
Diagnosing Scoliosis: Tests and Examinations
Diagnosis typically involves a physical examination to assess spinal curvature and asymmetry. Imaging tests such as X-rays provide detailed views of the spine to determine curvature severity. In some cases, MRI or CT scans are used to evaluate underlying causes or complications.

Treatment Options for Scoliosis Series
Treatment depends on curvature severity, age, and underlying cause. Mild cases may require regular monitoring. More severe cases might involve bracing to help straighten the spine, and in some instances, surgery may be necessary to correct and stabilize the curvature.
Non-Surgical Approaches to Managing Scoliosis
Non-surgical management focuses on preventing progression and managing symptoms. Options include physical therapy to improve posture, strengthen spinal muscles, and enhance flexibility. Chiropractic care, acupuncture, and specialized exercise programs may also be beneficial.

Surgical Interventions for Scoliosis
Surgical intervention is considered for severe or rapidly progressing scoliosis. Surgery aims to correct the curvature and stabilize the spine using techniques like spinal fusion, where vertebrae are fused together, and the use of rods, screws, or other devices for support.
Rehabilitation and Physical Therapy for Scoliosis
Rehabilitation and physical therapy are crucial for recovery and managing scoliosis. Therapy can improve strength, flexibility, and posture, and alleviate pain. Programs may include targeted exercises, manual therapy, and education on body mechanics and posture.

Living with Scoliosis: Coping Strategies and Support
Living with scoliosis can be challenging. Developing coping strategies and seeking support from healthcare professionals, family, and friends is important. Activities that promote physical and mental well-being, such as regular exercise, good posture, and counseling or support groups, can help manage the condition’s impact.
Prevention and Early Intervention for Scoliosis
Although scoliosis may not be entirely preventable, early intervention and regular monitoring can help manage the condition before it worsens. Regular check-ups, especially during adolescence, can detect early signs and allow timely intervention. Maintaining good posture, engaging in regular exercise, and avoiding excessive weight gain can support spinal health and reduce scoliosis risk.
Références
Société de recherche sur la scoliose. "Comprendre la scoliose". Scoliosis Research Journal.
Fong, D. “The Role of Genetics in Scoliosis.” Colonne vertébrale. 2019;44(12):910-918.

