Lordosis and scoliosis are two distinct spinal conditions that can affect individuals of all ages. While both conditions involve abnormal curvature of the spine, they differ in terms of their unique characteristics, causes, symptoms, and treatment options. Understanding the differences between lordosis and scoliosis is crucial for accurate diagnosis and effective management of these conditions. In this article, we will delve into the details of each condition, exploring their causes, risk factors, symptoms, diagnosis, treatment options, and potential complications.
What is Lordosis?
Lordosis, also known as swayback or hyperlordosis, is a condition characterized by an excessive inward curvature of the spine in the lower back. This abnormal curvature causes the buttocks to protrude and the abdomen to appear more prominent. Lordosis can affect individuals of all ages, but it is most commonly seen in children and adolescents during their growth spurts.

Causes and Risk Factors of Lordosis
There are several factors that can contribute to the development of lordosis. One of the primary causes is poor posture, particularly when sitting or standing for extended periods with the pelvis tilted forward. Other potential causes include obesity, pregnancy, certain neuromuscular conditions such as muscular dystrophy, and congenital abnormalities of the spine.
Certain risk factors may increase an individual’s likelihood of developing lordosis. These include a sedentary lifestyle, excessive weight gain, certain occupations that require prolonged sitting or standing, and certain medical conditions that affect muscle tone and strength.
Symptoms and Diagnosis of Lordosis
The most noticeable symptom of lordosis is an exaggerated inward curve of the lower back. This can lead to a protruding abdomen and buttocks. In some cases, individuals with lordosis may experience lower back pain, muscle stiffness, and difficulty standing for long periods. In severe cases, lordosis can also affect an individual’s gait and overall mobility.
To diagnose lordosis, a healthcare professional will typically perform a physical examination, assess the individual’s medical history, and may order imaging tests such as X-rays or MRI scans. These tests help determine the severity of the curvature and identify any underlying causes or complications.
Treatment Options for Lordosis
The treatment of lordosis depends on the severity of the condition and the presence of any underlying causes. In mild cases, lifestyle modifications such as maintaining good posture, engaging in regular exercise to strengthen the core muscles, and weight management may be sufficient to alleviate symptoms and prevent further progression.
For more severe cases, physical therapy may be recommended to improve muscle strength and flexibility. In some instances, a back brace may be prescribed to provide support and help correct the curvature. In rare cases where lordosis is causing significant pain or mobility issues, surgery may be considered to correct the curvature and stabilize the spine.
Complications and Long-term Effects of Lordosis
If left untreated, lordosis can lead to various complications and long-term effects. These may include chronic back pain, muscle imbalances, increased risk of spinal injuries, and decreased mobility. Additionally, severe lordosis can put excessive pressure on the spinal discs, leading to herniation or degeneration over time.
It is important to note that the long-term effects of lordosis can vary depending on the underlying cause, severity of the curvature, and individual factors. Regular monitoring and appropriate management are essential to prevent or minimize these potential complications.
Qu'est-ce que la scoliose ?
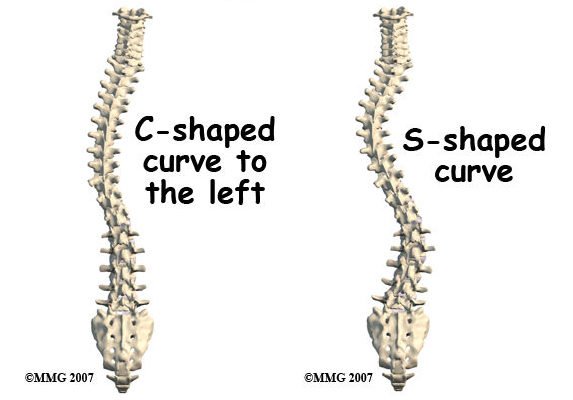
Scoliosis is a condition characterized by an abnormal sideways curvature of the spine. Instead of the spine appearing straight when viewed from the front or back, it may have an “S” or “C” shape. Scoliosis can affect individuals of all ages, but it most commonly develops during adolescence.
Causes and Risk Factors of Scoliosis
The exact cause of scoliosis is often unknown and is referred to as idiopathic scoliosis. However, certain risk factors have been identified. These include a family history of scoliosis, female gender (as scoliosis is more common in girls), rapid growth during adolescence, and certain neuromuscular conditions such as cerebral palsy or muscular dystrophy.
Symptoms and Diagnosis of Scoliosis
The symptoms of scoliosis can vary depending on the severity of the curvature. In mild cases, there may be no noticeable symptoms, while in more severe cases, individuals may experience back pain, muscle stiffness, and uneven shoulder or hip heights. In some instances, scoliosis can also affect an individual’s posture and overall appearance.
To diagnose scoliosis, a healthcare professional will typically perform a physical examination, assess the individual’s medical history, and may order imaging tests such as X-rays or MRI scans. These tests help determine the degree of curvature, identify any underlying causes, and guide treatment decisions.
Options de traitement de la scoliose
The treatment of scoliosis depends on several factors, including the severity of the curvature, the individual’s age, and the presence of any underlying conditions. In mild cases, regular monitoring may be sufficient, with no specific treatment required. However, individuals with moderate to severe scoliosis may require intervention to prevent further progression and manage symptoms.
One common treatment option for scoliosis is the use of braces. These braces are designed to apply pressure to the spine and help correct the curvature. Bracing is typically recommended for individuals who are still growing and have a curvature between 25 and 45 degrees. Physical therapy may also be prescribed to improve muscle strength and flexibility.
In cases where the curvature is severe or rapidly progressing, surgery may be considered. Spinal fusion surgery is the most common surgical procedure for scoliosis. It involves fusing the vertebrae together using metal rods, screws, or hooks to straighten the spine and prevent further curvature.
Complications and Long-term Effects of Scoliosis
If left untreated, scoliosis can lead to various complications and long-term effects. These may include chronic back pain, respiratory problems due to reduced lung capacity, decreased mobility, and psychological effects such as self-esteem issues. Additionally, severe scoliosis can put excessive pressure on the spinal discs, leading to herniation or degeneration over time.
Regular monitoring and appropriate management are crucial to prevent or minimize these potential complications. It is important to note that the long-term effects of scoliosis can vary depending on the severity of the curvature, the age of onset, and individual factors.
Conclusion
Lordosis and scoliosis are two distinct spinal conditions that involve abnormal curvature of the spine. While lordosis is characterized by an excessive inward curvature of the lower back, scoliosis involves an abnormal sideways curvature. Understanding the unique characteristics, causes, symptoms, diagnosis, treatment options, and potential complications of each condition is essential for accurate diagnosis and effective management.
Both lordosis and scoliosis can have significant impacts on an individual’s quality of life if left untreated. Therefore, early detection, appropriate treatment, and regular monitoring are crucial to prevent further progression, manage symptoms, and minimize potential complications. By raising awareness and promoting understanding of these conditions, we can ensure that individuals with lordosis or scoliosis receive the care and support they need to lead healthy and fulfilling lives.
Références
- Smith, J.R., & McCarthy, R.E. “Lordosis and its clinical implications.” Spine (Phila Pa 1976). 2009;34(10):1050-1057. doi: 10.1097/BRS.0b013e3181a13f6b.
- Weinstein, S.L., Dolan, L.A., Cheng, J.C., Danielsson, A., & Morcuende, J.A. “Adolescent idiopathic scoliosis.” The Lancet. 2008;371(9623):1527-1537. doi : 10.1016/S0140-6736(08)60658-3.
- Sato, K., & Kikuchi, S. “Lordosis and its effects on the spine.” Cliniques orthopédiques d'Amérique du Nord. 2011;42(4):543-550. doi: 10.1016/j.ocl.2011.07.002.
- Negrini, S., Donzelli, S., Aulisa, A.G., et al. “2016 SOSORT guidelines: orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth.” Scoliose et troubles de la colonne vertébrale. 2018;13:3. doi : 10.1186/s13013-017-0145-8.
- Danielsson, A.J., Nachemson, A.L. “Childhood and adolescent scoliosis and the effect of bracing.” Spine (Phila Pa 1976). 2001;26(18):2006-2012. doi: 10.1097/00007632-200109150-00016.
- Balagué, F., Pellisé, F., & Aebi, M. “Idiopathic scoliosis.” Best Practice & Research Clinical Rheumatology. 2007;21(2):227-239. doi: 10.1016/j.berh.2006.12.002.
- Weinstein, S.L., Zavala, D.C., Ponseti, I.V. “Idiopathic scoliosis: long-term follow-up and prognosis in untreated patients.” Le journal de la chirurgie osseuse et articulaire. 1981;63(5):702-712. doi : 10.2106/00004623-198163050-00004.
- Mac-Thiong, J.M., Transfeldt, E.E., Parent, S., Labelle, H. “Surgical correction of lordosis in spinal deformities.” Spine (Phila Pa 1976). 2012;37(19):1593-1601. doi: 10.1097/BRS.0b013e318251892b.
- Cheng, J.C., Castelein, R.M., Chu, W.C., et al. “Adolescent idiopathic scoliosis.” Nature Reviews Disease Primers (en anglais). 2015;1:15030. doi: 10.1038/nrdp.2015.30.
- Danielsson, A.J., Hasserius, R., Ohlin, A., Nachemson, A.L. “Scoliosis in the adult: results of surgery.” Spine (Phila Pa 1976). 2007;32(3):302-310. doi: 10.1097/01.brs.0000254282.30943.8b.
- Reamy, B.V., Slakey, J.B. “Adolescent idiopathic scoliosis: review and current concepts.” American Family Physician (en anglais). 2001;64(1):111-116. doi : 10.1007/s10437-005-0002-7.
- Weiss, H.R., Lehnert-Schroth, C., Moramarco, M. “The Schroth method of scoliosis treatment: review of the literature.” Studies in Health Technology and Informatics. 2012;176:303-306. doi: 10.3233/978-1-60750-961-7-303.
- Yanik, E.L., Becker, A.C., Lungren, M.P., et al. “MRI assessment of spine deformity in pediatric scoliosis.” Journal of Magnetic Resonance Imaging. 2021;53(5):1352-1363. doi: 10.1002/jmri.27314.
- Smith, J.S., Klineberg, E., Schwab, F.J., et al. “Prospective multicenter assessment of perioperative and minimum 2-year postoperative complication rates associated with adult spinal deformity surgery.” Journal of Neurosurgery : Colonne vertébrale. 2017;26(6):730-740. doi: 10.3171/2016.10.SPINE16334.
- Bunnell, W.P. “The natural history of idiopathic scoliosis before skeletal maturity.” Spine (Phila Pa 1976). 1986;11(8):773-776. doi : 10.1097/00007632-198610000-00006.

