Scoliosis is a condition characterized by an abnormal curvature of the spine. While most cases of scoliosis are mild and do not cause significant health issues, it is crucial to identify and monitor any signs of spinal deformity, even in minor cases. Early detection and intervention can prevent the progression of scoliosis and minimize potential complications. Interpreting a minor scoliosis X-ray is an essential step in recognizing early signs of spinal deformity and ensuring appropriate treatment. In this article, we will explore the key components of scoliosis X-rays and discuss how to interpret them accurately.

Understanding the basics of scoliosis X-rays
Scoliosis X-rays, also known as spinal radiographs, are diagnostic imaging tests that provide a detailed view of the spine’s structure. These X-rays are crucial in assessing the severity and progression of scoliosis. They help healthcare professionals determine the appropriate treatment plan and monitor the effectiveness of interventions.
Identifying the key components of a scoliosis X-ray
To interpret a scoliosis X-ray accurately, it is essential to identify the key components. These include the spine’s curvature, the degree of spinal rotation, the location and direction of the spinal curve, and the Cobb angle measurement.
Analyzing the curvature of the spine in an X-ray
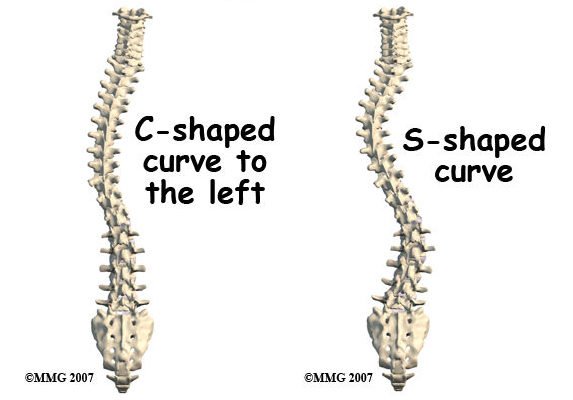
When examining a scoliosis X-ray, the curvature of the spine is one of the primary aspects to assess. The spine should appear straight when viewed from the front or back. However, in scoliosis, the spine may curve sideways, forming an “S” or “C” shape. Analyzing the curvature helps determine the severity of scoliosis and the appropriate treatment approach.
Recognizing the degree of spinal rotation in X-rays
In addition to the curvature, the degree of spinal rotation is another crucial factor to consider. Scoliosis can cause the vertebrae to rotate, leading to a visible rib hump or prominence on one side of the back. Assessing the degree of spinal rotation helps determine the severity of scoliosis and guides treatment decisions.
Assessing the location and direction of the spinal curve
The location and direction of the spinal curve are essential in understanding the impact of scoliosis on the body. The curve can occur in different regions of the spine, such as the thoracic (upper back), lumbar (lower back), or both. Additionally, the curve can be either to the left (levoscoliosis) or to the right (dextroscoliosis). Evaluating the location and direction of the spinal curve aids in determining the appropriate treatment plan.
Evaluating the severity of scoliosis based on X-ray findings
Interpreting a scoliosis X-ray involves evaluating the severity of the condition. Healthcare professionals use various methods to assess severity, including measuring the Cobb angle, which is the most common method. The Cobb angle measures the angle between the most tilted vertebrae at the top and bottom of the curve. A higher Cobb angle indicates a more severe curvature and may require more aggressive treatment.
Interpreting the Cobb angle measurement in X-rays
The Cobb angle measurement is crucial in determining the severity of scoliosis. A Cobb angle of less than 10 degrees is considered within the normal range, while an angle between 10 and 25 degrees indicates mild scoliosis. Moderate scoliosis is defined by a Cobb angle between 25 and 40 degrees, and severe scoliosis is characterized by a Cobb angle greater than 40 degrees. Interpreting the Cobb angle measurement helps guide treatment decisions and monitor the progression of scoliosis over time.

Identifying potential complications or associated conditions
While interpreting a minor scoliosis X-ray, it is essential to be aware of potential complications or associated conditions. Scoliosis can sometimes be associated with other health issues, such as congenital abnormalities, neuromuscular disorders, or connective tissue disorders. Identifying these conditions is crucial for comprehensive treatment planning and ensuring the best possible outcomes for patients.
Differentiating between structural and non-structural scoliosis
When interpreting a scoliosis X-ray, it is important to differentiate between structural and non-structural scoliosis. Structural scoliosis involves a fixed curvature of the spine, while non-structural scoliosis is reversible and caused by factors such as muscle imbalances or leg length discrepancies. Differentiating between these types of scoliosis helps determine the appropriate treatment approach.
Recognizing early signs of spinal deformity in X-rays
Interpreting a minor scoliosis X-ray requires a keen eye for early signs of spinal deformity. These signs may include a slight curvature of the spine, mild rotation of the vertebrae, or a small rib hump. While these signs may be subtle, they should not be overlooked, as early intervention can prevent the progression of scoliosis and minimize potential complications.
Seeking professional medical advice for accurate diagnosis and treatment
Interpreting a minor scoliosis X-ray is a complex task that requires expertise and experience. While this article provides a general overview, it is crucial to seek professional medical advice for accurate diagnosis and treatment. A qualified healthcare professional, such as an orthopedic specialist or a spine surgeon, can thoroughly evaluate the X-ray findings, consider the patient’s medical history, and recommend the most appropriate treatment plan.
In conclusion, interpreting a minor scoliosis X-ray is a crucial step in recognizing early signs of spinal deformity. Understanding the key components of scoliosis X-rays, such as the curvature of the spine, the degree of spinal rotation, the location and direction of the spinal curve, and the Cobb angle measurement, helps healthcare professionals assess the severity of scoliosis and guide treatment decisions. By recognizing early signs of spinal deformity and seeking professional medical advice, individuals with scoliosis can receive timely interventions and achieve the best possible outcomes for their spinal health.
References
- Youssef, J. A., et al. “Current Status of Adult Spinal Deformity.” Global Spine Journal, vol. 3, no. 1, 2013, pp. 51-62. doi: 10.1055/s-0032-1326956
- Nash, C. L., & Moe, J. H. “A Study of Vertebral Rotation.” The Journal of Bone and Joint Surgery. American Volume, vol. 51, no. 2, 1969, pp. 223-229. doi: 10.2106/00004623-196951020-00004
- Morrissy, R. T., et al. “Measurement of the Cobb angle on radiographs of patients who have scoliosis.” The Journal of Bone and Joint Surgery. American Volume, vol. 72, no. 3, 1990, pp. 320-327. doi: 10.2106/00004623-199072030-00010
- Weinstein, S. L., et al. “The Natural History of Adolescent Idiopathic Scoliosis.” The Journal of Bone and Joint Surgery. American Volume, vol. 65, no. 4, 1983, pp. 447-455. doi: 10.2106/00004623-198365040-00012
- Scherl, S. A., & Johnston, C. E. “Idiopathic scoliosis: current concepts and techniques.” Orthopedic Clinics of North America, vol. 35, no. 3, 2004, pp. 247-258. doi: 10.1016/j.ocl.2004.01.001
- Scoliosis Research Society (SRS). “Scoliosis Diagnosis and Treatment.” Scoliosis Research Society, 2020. Available at: www.srs.org
- Lonstein, J. E., & Carlson, J. M. “The prediction of curve progression in untreated idiopathic scoliosis during growth.” The Journal of Bone and Joint Surgery. American Volume, vol. 66, no. 7, 1984, pp. 1061-1071. doi: 10.2106/00004623-198466070-00013
- Weinstein, S. L., et al. “Effect of bracing in adolescents with idiopathic scoliosis.” The New England Journal of Medicine, vol. 369, no. 16, 2013, pp. 1512-1521. doi: 10.1056/NEJMoa1307337
- Richards, B. S., & Vitale, M. G. “The diagnosis and treatment of pediatric scoliosis.” Journal of the American Academy of Orthopaedic Surgeons, vol. 16, no. 4, 2008, pp. 211-222. doi: 10.5435/00124635-200804000-00004
- Karol, L. A. “The natural history of scoliosis and the indications for surgical intervention.” Spine (Phila Pa 1976), vol. 28, no. 20, 2003, pp. S97-S104. doi: 10.1097/01.BRS.0000090420.61583.ED
- Negrini, S., et al. “Scoliosis-specific exercises for treatment of adolescent idiopathic scoliosis: a comprehensive review.” European Journal of Physical and Rehabilitation Medicine, vol. 55, no. 6, 2019, pp. 714-736. doi: 10.23736/S1973-9087.19.05894-7
- Fadzan, M., & Bettany-Saltikov, J. “The evidence for conservative management of adolescent idiopathic scoliosis (AIS): current trends and future directions.” Healthcare (Basel), vol. 6, no. 3, 2018, pp. 81. doi: 10.3390/healthcare6030081
- Schlosser, T. P., et al. “Surgical versus non-surgical treatment of primary scoliosis in children: a systematic review and meta-analysis.” Spine (Phila Pa 1976), vol. 40, no. 16, 2015, pp. 1283-1293. doi: 10.1097/BRS.0000000000001025
- Cobb, J. R. “Outline for the study of scoliosis.” American Academy of Orthopedic Surgeons Instructional Course Lectures, 1948, vol. 5, pp. 261-275.
- Hawes, M. C. “Impact of spine surgery on signs and symptoms of spinal deformity.” Pediatric Rehabilitation, vol. 9, no. 4, 2006, pp. 318-339. doi: 10.1080/13638490500402427

