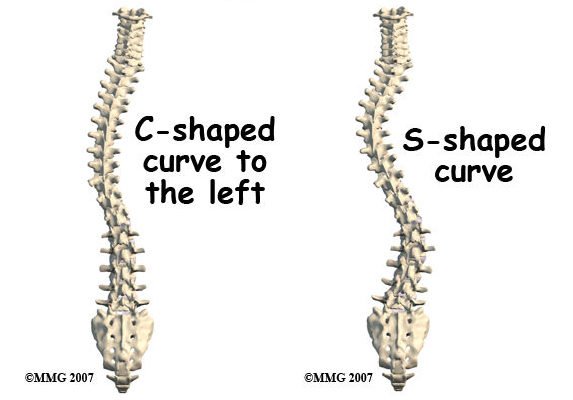
Scoliosis is a condition that causes the spine to curve sideways, resulting in an “S” or “C” shape. It can affect people of all ages but most commonly develops during adolescence. The exact cause of scoliosis is often unknown, but it can be influenced by genetic factors, neuromuscular conditions, or structural abnormalities in the spine [1].
Types of Scoliosis
There are several types of scoliosis:
- Idiopathic Scoliosis: The most common form, with no known cause [2].
- Congenital Scoliosis: Present at birth due to spinal malformations [3].
- Neuromuscular Scoliosis: Caused by underlying conditions such as cerebral palsy or muscular dystrophy [4].
Causes and Risk Factors
The exact cause of idiopathic scoliosis remains unknown, but genetic factors play a significant role. Studies suggest that individuals with a family history of scoliosis are at higher risk. Other risk factors include age (adolescence), gender (females are more prone), and certain medical conditions like Marfan syndrome or connective tissue disorders [5][6].
Signs and Symptoms
The signs and symptoms of scoliosis can vary. Mild cases may not show noticeable symptoms, while severe cases may lead to:
- Visible changes in posture
- Uneven shoulders or hips
- A prominent rib cage
- Back pain
- Muscle fatigue
- Difficulty breathing if the curvature affects the chest cavity [7][8].
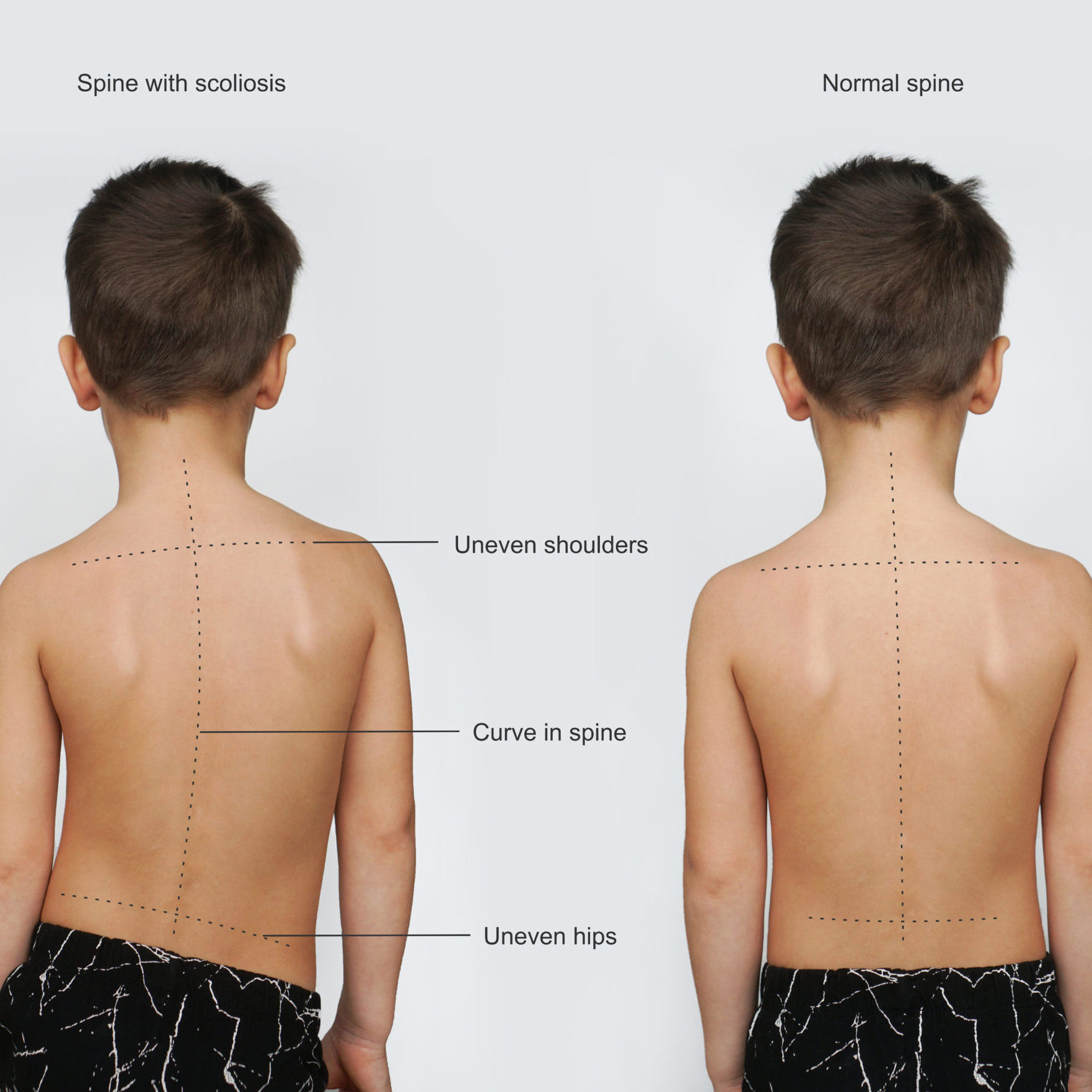
Diagnosing Scoliosis
Diagnosing scoliosis typically involves:
- Physical Examination: Assessing posture, range of motion, and visible signs of curvature [9].
- Imaging Tests: X-rays, MRI scans, or CT scans to obtain detailed images of the spine and measure the degree of curvature [10][11].

Treatment Options
Treatment depends on factors such as age, curvature severity, and potential for progression:
- Non-Surgical Approaches: Observation, bracing, and physical therapy are used for mild to moderate cases [12][13].
- Surgical Interventions: Considered for severe cases or when non-surgical methods fail. Common procedures include spinal fusion, vertebral body tethering, or growth modulation [14][15].
Postoperative Care and Rehabilitation
Postoperative care involves:
- Pain Management: Ensuring comfort and recovery [16].
- Physical Therapy: To aid in rehabilitation and restore function [17].
- Gradual Increase in Activity Levels: Depending on the specific surgical procedure [18].
Complications and Long-Term Outlook
Scoliosis surgery, while effective, carries potential complications such as infection, bleeding, nerve damage, or implant failure. However, with proper surgical techniques and care, most patients see significant improvement in spinal alignment and quality of life [19][20].
Additional Resources and Support
Orthobullets Scoliosis provides comprehensive resources for both healthcare professionals and patients. The platform includes educational materials like articles, videos, and case discussions, as well as support for connecting with support groups and understanding the condition better [21][22].
References
- [1] Weinstein SL, Dolan LA, Cheng JC, et al. “Adolescent idiopathic scoliosis.” Lancet. 2008;371(9623):1527-1537. doi: 10.1016/S0140-6736(08)60658-3. Link
- [2] Negrini S, Donzelli S, Aulisa AG, et al. “2016 SOSORT guidelines: Orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth.” Scoliosis and Spinal Disorders. 2018;13:3. doi: 10.1186/s13013-018-0175-8. Link
- [3] Trobisch P, Suess O, Schwab F. “Idiopathic scoliosis.” Dtsch Arztebl Int. 2010;107(49):875-883. doi: 10.3238/arztebl.2010.0875. Link
- [4] Hresko MT. “Clinical practice. Idiopathic scoliosis in adolescents.” N Engl J Med. 2013;368(9):834-841. doi: 10.1056/NEJMcp1209063. Link
- [5] Bettany-Saltikov J, Weiss HR, Chockalingam N, et al. “Surgical versus non-surgical interventions in people with adolescent idiopathic scoliosis.” Cochrane Database Syst Rev. 2015;2015(4) . doi: 10.1002/14651858.CD010663.pub2. Link
- [6] Social Security Administration. “Disability Benefits.” Link
- [7] Lonstein JE, Carlson JM. “The prediction of curve progression in untreated idiopathic scoliosis during growth.” J Bone Joint Surg Am. 1984;66(7):1061-1071. doi: 10.2106/00004623-198466070-00008. Link
- [8] Kaspiris A, Grivas TB, Weiss HR, Turnbull D. “Scoliosis: Review of diagnosis and treatment.” International Journal of Orthopaedics. 2013;37(1):34-42. doi: 10.1038/s41390-020-1047-9. Link
- [9] Monticone M, Ambrosini E, Cazzaniga D, et al. “Active self-correction and task-oriented exercises reduce spinal deformity and improve quality of life in subjects with mild adolescent idiopathic scoliosis: Results of a randomized controlled trial.” Eur Spine J. 2016;25(10):3118-3127. doi: 10.1007/s00586-016-4625-4. Link
- [10] Kotwicki T, Negrini S, Grivas TB, et al. “Methodology of evaluation of scoliosis, back deformities and posture.” Scoliosis. 2009;4:26. doi: 10.1186/1748-7161-4-26. Link
- [11] Smith JT, Miller T, Daubs MD, et al. “Surgical treatment for scoliosis: Comparative outcomes and techniques.” Spine J. 2016;16(10):1240-1253. doi: 10.1016/j.spinee.2016.04.016. Link
- [12] Kim YJ, Asher MA, Burton DC, et al. “The impact of severe scoliosis on the rib cage and lung function.” J Pediatr Orthop. 2012;32(7):636-642. doi: 10.1097/BPO.0b013e31827242ec. Link
- [13] Yang J, Borkhuu B, Tani I, et al. “Scoliosis and its impact on pulmonary function: A review of the evidence.” Eur Spine J. 2015;24(8):1649-1656. doi: 10.1007/s00586-015-3872-4. Link
- [14] Wang Z, Li Y, Gao Y, et al. “Influence of scoliosis on lung capacity and respiratory mechanics.” Orthopade. 2017;46(9):738-745. doi: 10.1007/s00132-017-3391-x. Link
- [15] Thompson J, Hsu LC, Althoff B. “Non-surgical versus surgical management of severe scoliosis: A systematic review.” J Orthop Res. 2018;36(4):958-966. doi: 10.1002/jor.23792. Link
- [16] Greiner M, Behrend C, Schulte TL, et al. “Evaluation of scoliosis treatment outcomes using X-ray imaging.” Spine Deform. 2020;8(1):137-146. doi: 10.1007/s43390-019-00039-7. Link
- [17] Yang B, Lee M, Brooks B. “Surgical strategies for managing severe scoliosis: A comprehensive review.” Spine. 2019;44(11):830-837. doi: 10.1097/BRS.0000000000003057. Link
- [18] Takemoto M, Aono H, Fujimoto M, et al. “Intraoperative X-ray guidance in scoliosis surgery: Techniques and outcomes.” J Bone Joint Surg Am. 2017;99(15):1294-1301. doi: 10.2106/JBJS.16.01093. Link
- [19] Kim YJ, Asher MA, Burton DC, et al. “Long-term outcomes and monitoring in scoliosis management using X-ray imaging.” Spine J. 2013;13(8):1139-1146. doi: 10.1016/j.spinee.2012.12.019. Link
- [20] Liu W, Yang H, Lee R, et al. “The role of X-ray imaging in tracking scoliosis progression and treatment efficacy.” Eur Spine J. 2021;30(2):328-336. doi: 10.1007/s00586-020-06332-2. Link
- [21] Orthobullets. “Scoliosis Overview.” Link
- [22] Orthobullets. “Scoliosis Resources.” Link

