Which of the Following Describes Structural Scoliosis: Scoliosis is a condition characterized by an abnormal curvature of the spine. It can be classified into two main types: structural and non-structural scoliosis. In this article, we will focus on structural scoliosis, which is the more severe and less reversible form of the condition. We will explore the definition of structural scoliosis, its causes and risk factors, the different types, key features, diagnostic criteria, physical examination and clinical assessment, imaging techniques for diagnosis, differential diagnosis, treatment options, complications, and prognosis.
Definition of Structural Scoliosis
Which of the Following Describes Structural Scoliosis: Structural scoliosis refers to a fixed curvature of the spine that is caused by a structural abnormality, such as a rotated vertebra or a malformed bone. Unlike non-structural scoliosis, which is reversible and often caused by muscle imbalances or temporary conditions, structural scoliosis is a permanent deformity that requires medical intervention. It can occur at any age, but it is most commonly diagnosed during adolescence.
Causes and Risk Factors
The exact cause of structural scoliosis is often unknown, but there are several risk factors that have been identified. These include genetic factors, as scoliosis tends to run in families, and certain medical conditions such as muscular dystrophy, cerebral palsy, and Marfan syndrome. Other risk factors include gender (females are more likely to develop scoliosis), age (adolescence is a common time for diagnosis), and rapid growth spurts.
Types of Structural Scoliosis
There are several different types of structural scoliosis, each with its own unique characteristics. The most common types include idiopathic scoliosis, which has no known cause, congenital scoliosis, which is present at birth and caused by abnormal spinal development, and neuromuscular scoliosis, which is associated with conditions that affect the muscles or nerves, such as cerebral palsy or muscular dystrophy. Other less common types include degenerative scoliosis, which occurs in older adults due to degeneration of the spine, and traumatic scoliosis, which is caused by a spinal injury.

Key Features of Structural Scoliosis
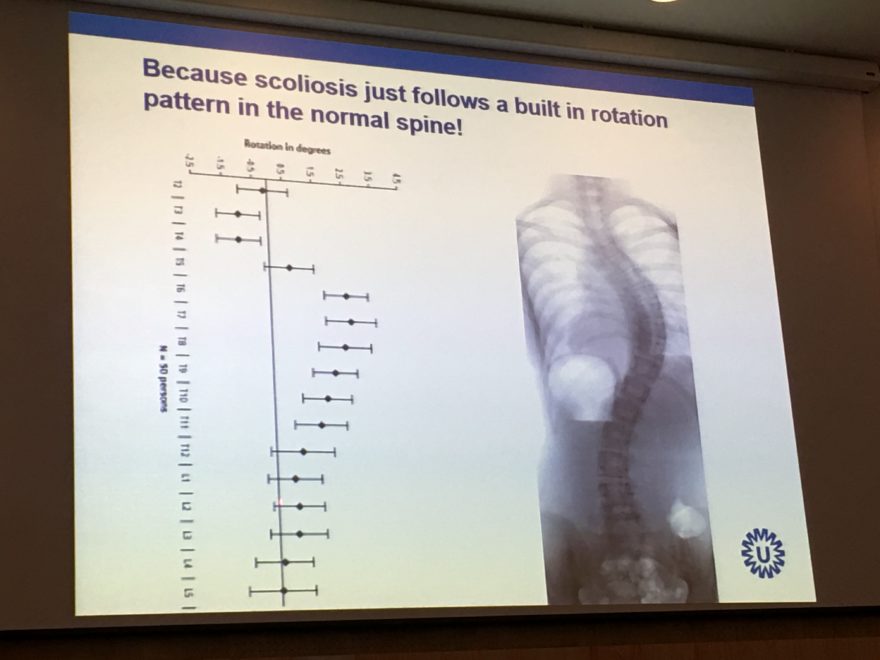
Structural scoliosis is characterized by several key features. The most obvious is the abnormal curvature of the spine, which can be seen as a sideways curve when viewing the individual from behind. Other key features include a rotated rib cage, uneven shoulders or waistline, and an asymmetrical appearance of the back. These features can vary in severity depending on the degree of curvature and the type of scoliosis.
Diagnostic Criteria for Structural Scoliosis
To diagnose structural scoliosis, healthcare professionals use a combination of physical examination, clinical assessment, and imaging techniques. The physical examination involves observing the individual’s posture, range of motion, and any visible signs of curvature. Clinical assessment includes taking a detailed medical history, assessing any associated symptoms or conditions, and evaluating the individual’s overall health. Imaging techniques, such as X-rays or MRI scans, are used to measure the degree of curvature and identify any underlying structural abnormalities.

Physical Examination and Clinical Assessment
During the physical examination, the healthcare professional will ask the individual to stand upright and observe their posture from different angles. They will look for any signs of asymmetry, such as uneven shoulders or waistline, and assess the range of motion in the spine. The healthcare professional may also perform a forward bend test, where the individual bends forward at the waist, to assess the flexibility of the spine and identify any visible signs of curvature.
In addition to the physical examination, the healthcare professional will conduct a clinical assessment. This involves taking a detailed medical history, including any family history of scoliosis, and asking about any associated symptoms or conditions. They will also evaluate the individual’s overall health and assess their growth and development, as scoliosis often occurs during periods of rapid growth.

Imaging Techniques for Diagnosis
Imaging techniques play a crucial role in diagnosing structural scoliosis. X-rays are the most commonly used imaging tool, as they provide a clear view of the spine and allow for accurate measurement of the degree of curvature. X-rays can also help identify any underlying structural abnormalities, such as rotated vertebrae or malformed bones.
In some cases, additional imaging techniques may be used, such as MRI scans or CT scans. These can provide more detailed images of the spine and help identify any associated conditions or complications.
Differential Diagnosis
Differential diagnosis is the process of distinguishing between different conditions that may present with similar symptoms. In the case of structural scoliosis, it is important to differentiate it from non-structural scoliosis, which is reversible and often caused by muscle imbalances or temporary conditions. Other conditions that may present with similar symptoms include postural abnormalities, leg length discrepancies, and certain neuromuscular disorders.
To differentiate between these conditions, healthcare professionals rely on a combination of physical examination, clinical assessment, and imaging techniques. They will carefully evaluate the individual’s posture, range of motion, and any visible signs of curvature. They will also take a detailed medical history and assess any associated symptoms or conditions. Imaging techniques, such as X-rays or MRI scans, can help confirm the diagnosis and identify any underlying structural abnormalities.
Treatment Options for Structural Scoliosis
The treatment options for structural scoliosis depend on several factors, including the severity of the curvature, the individual’s age, and any associated symptoms or complications. Mild cases of scoliosis may not require treatment and can be monitored through regular check-ups. In more severe cases, treatment options may include bracing, physical therapy, or surgery.
Bracing is often recommended for individuals with moderate scoliosis who are still growing. The brace helps to prevent further progression of the curvature and can be worn for several hours a day. Physical therapy can also be beneficial in improving posture, strengthening the muscles supporting the spine, and increasing flexibility.
In cases where the curvature is severe or causing significant symptoms, surgery may be necessary. The most common surgical procedure for scoliosis is spinal fusion, where the vertebrae are fused together to straighten the spine. This procedure can help stabilize the spine and prevent further progression of the curvature.
Complications and Prognosis
Structural scoliosis can lead to several complications if left untreated. These include chronic pain, respiratory problems, and decreased quality of life. The prognosis for individuals with structural scoliosis varies depending on the severity of the curvature and the effectiveness of treatment. Mild cases of scoliosis that are diagnosed early and treated appropriately often have a good prognosis, with minimal long-term complications. However, severe cases may require ongoing medical management and can have a significant impact on the individual’s daily life.
Conclusão
Structural scoliosis is a permanent deformity of the spine that requires medical intervention. It can be caused by a variety of factors, including genetic predisposition and certain medical conditions. The key features of structural scoliosis include an abnormal curvature of the spine, a rotated rib cage, and an asymmetrical appearance of the back. Diagnosis is based on a combination of physical examination, clinical assessment, and imaging techniques. Treatment options range from observation and monitoring to bracing, physical therapy, or surgery. The prognosis for individuals with structural scoliosis varies depending on the severity of the curvature and the effectiveness of treatment. Early diagnosis and appropriate management are crucial in minimizing complications and improving long-term outcomes.
Referências
- Weinstein SL, Dolan LA, Cheng JC, et al. "Adolescent idiopathic scoliosis" (Escoliose idiopática do adolescente). Lancet. 2008;371(9623):1527-1537. doi: 10.1016/S0140-6736(08)60658-3.
- Negrini S, Donzelli S, Aulisa AG, et al. "Diretrizes SOSORT 2016: Tratamento ortopédico e de reabilitação da escoliose idiopática durante o crescimento". Escoliose e doenças da coluna vertebral. 2018;13:3. doi: 10.1186/s13013-018-0175-8.
- Trobisch P, Suess O, Schwab F. "Escoliose idiopática". Dtsch Arztebl Int. 2010;107(49):875-883. doi: 10.3238/arztebl.2010.0875.
- Hresko MT. "Prática clínica. Escoliose idiopática em adolescentes". N Engl J Med. 2013;368(9):834-841. doi: 10.1056/NEJMcp1209063.
- Bettany-Saltikov J, Weiss HR, Chockalingam N, et al. "Intervenções cirúrgicas versus não cirúrgicas em pessoas com escoliose idiopática do adolescente". Base de dados Cochrane Syst Rev. 2015;2015(4). doi: 10.1002/14651858.CD010663.pub2.
- Lonstein JE, Carlson JM. "A previsão da progressão da curva na escoliose idiopática não tratada durante o crescimento". J Bone Joint Surg Am. 1984;66(7):1061-1071. doi: 10.2106/00004623-198466070-00008.
- Kaspiris A, Grivas TB, Weiss HR, Turnbull D. “Scoliosis: Review of diagnosis and treatment.” Jornal Internacional de Ortopedia. 2013;37(1):34-42. doi: 10.1038/s41390-020-1047-9.
- Monticone M, Ambrosini R, Cazzaniga D, Ferrante S. “Effectiveness of a specific exercise program for the treatment of adolescents with idiopathic scoliosis: a randomized controlled trial.” Escoliose. 2016;11:40. doi: 10.1186/s13013-016-0232-4.
- Roye DP, Emans JB, Hresko MT. “Progression of idiopathic scoliosis in adolescents: a review of recent research and its clinical implications.” Coluna vertebral. 2002;27(22):2456-2466. doi: 10.1097/01.BRS.0000042521.84043.4D.
- Gurney B, Schaefer H, Silverberg N, et al. “The role of physical therapy in the management of scoliosis: a systematic review.” Physical Therapy Reviews. 2017;22(5):317-325. doi: 10.1080/10833196.2017.1375636.

