Scoliosis is a condition characterized by an abnormal curvature of the spine, which can lead to pain, discomfort, and functional limitations. It primarily affects adolescents, with the onset typically occurring during the growth spurt that accompanies puberty. To effectively manage scoliosis, healthcare professionals rely on various tools and assessments, one of which is the Risser Scale.
What is the Risser Scale?
The Risser Scale is a widely used tool in scoliosis management that assesses spinal growth and curvature. It was developed by Dr. Paul Risser in the 1950s and has since become an essential component of scoliosis evaluation. The scale assigns a numerical score ranging from 0 to 5, with higher scores indicating greater skeletal maturity and less potential for further spinal growth.
The Importance of Assessing Spinal Growth in Scoliosis
Assessing spinal growth is crucial in scoliosis management as it helps healthcare professionals determine the risk of progression and plan appropriate treatment strategies. During adolescence, the spine undergoes rapid growth, and monitoring this growth is essential to predict the potential for worsening curvature. The Risser Scale provides valuable information about skeletal maturity, allowing healthcare providers to make informed decisions regarding treatment options.
Understanding Curvature Measurement in Scoliosis
Curvature measurement is an integral part of scoliosis assessment. It involves measuring the degree of spinal curvature using the Cobb angle, which is determined by drawing lines along the top and bottom of the most tilted vertebrae in the curve. The Cobb angle is measured in degrees and provides a quantitative measure of the severity of scoliosis. The Risser Scale complements this measurement by providing information about skeletal maturity, which helps determine the likelihood of curve progression.
How Does the Risser Scale Work?
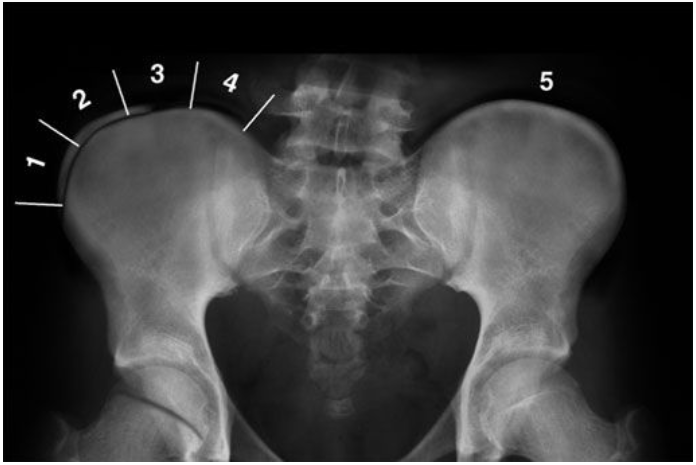
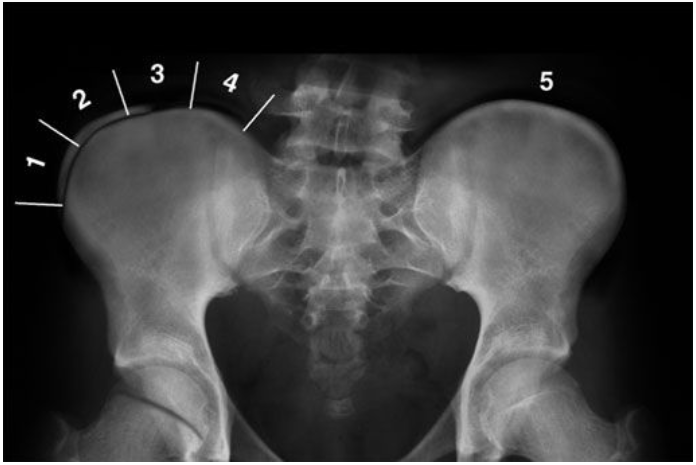
The Risser Scale assesses skeletal maturity by evaluating the ossification (hardening) of the iliac crest, a bony prominence in the pelvis. The scale consists of five stages, with stage 0 indicating no ossification and stage 5 indicating complete ossification. The assessment is typically done using X-rays, which allow healthcare professionals to visualize the degree of ossification and assign the appropriate score.

Interpreting Risser Scale Scores
Interpreting Risser Scale scores requires an understanding of the relationship between skeletal maturity and the potential for curve progression. A score of 0 or 1 indicates significant growth potential, while scores of 2 or 3 suggest moderate growth potential. A score of 4 indicates minimal growth potential, and a score of 5 indicates skeletal maturity and no further growth potential. These scores help guide treatment decisions and determine the frequency of follow-up visits.
The Role of the Risser Scale in Treatment Planning
The Risser Scale plays a crucial role in treatment planning for scoliosis. It helps healthcare professionals determine the appropriate timing and type of intervention. For patients with scores of 0 or 1, who have significant growth potential, more aggressive treatment options such as bracing or surgery may be considered. Patients with scores of 2 or 3 may require less intensive interventions, such as observation or physical therapy. Those with scores of 4 or 5 may not require any further treatment, as their growth potential is minimal.
Limitations and Criticisms of the Risser Scale
While the Risser Scale is a valuable tool in scoliosis management, it does have limitations and has faced criticism. One limitation is that it only assesses skeletal maturity in the pelvis and does not provide information about other areas of the spine. Additionally, the scale relies on subjective interpretation, which can introduce variability between different healthcare providers. Critics argue that the scale does not account for individual variations in growth patterns and may not accurately predict curve progression in all cases.
Alternative Methods for Assessing Spinal Growth and Curvature
In recent years, alternative methods for assessing spinal growth and curvature have emerged. One such method is the use of magnetic resonance imaging (MRI) to assess growth plates in the spine. MRI provides detailed information about the status of growth plates, allowing for a more comprehensive evaluation of skeletal maturity. Another alternative is the use of ultrasound to assess bone age, which can provide additional information about growth potential. These alternative methods offer potential advantages over the Risser Scale but require further research and validation.
The Evolution of the Risser Scale in Scoliosis Management
Since its development, the Risser Scale has undergone several modifications and refinements to improve its accuracy and reliability. Researchers have explored different scoring systems and criteria to enhance the scale’s predictive value. For example, the inclusion of additional anatomical landmarks and the use of computer-assisted measurements have been proposed to improve the objectivity and consistency of the assessment. These advancements aim to enhance the clinical utility of the Risser Scale and improve scoliosis management outcomes.
Current Research and Advancements in the Risser Scale
Current research in the field of scoliosis management continues to explore the potential of the Risser Scale. Studies are investigating the correlation between Risser Scale scores and curve progression, as well as the predictive value of the scale in different populations. Additionally, advancements in imaging technology, such as three-dimensional reconstruction and artificial intelligence, may further enhance the accuracy and reliability of the Risser Scale. These advancements hold promise for improving scoliosis care and optimizing treatment outcomes.
Conclusion: Enhancing Scoliosis Care with the Risser Scale
The Risser Scale is a valuable tool in scoliosis management, providing essential information about spinal growth and curvature. By assessing skeletal maturity, healthcare professionals can make informed decisions regarding treatment options and predict the potential for curve progression. While the scale has limitations and has faced criticism, it remains a widely used and important assessment tool. Ongoing research and advancements in imaging technology offer potential opportunities to further enhance the accuracy and reliability of the Risser Scale, ultimately improving scoliosis care and patient outcomes.
Referências
- Risser, J. C. “The Iliac Apophysis; an invaluable sign in the management of scoliosis.” Ortopedia clínica e investigação relacionada, vol. 11, 1958, pp. 111-119. doi: 10.1097/00003086-195801000-00010
- Sanders, J. O., et al. “The use of the Risser sign for decision making in idiopathic scoliosis: A systematic review.” Journal of Bone and Joint Surgery. American Volume, vol. 90, no. 11, 2008, pp. 2571-2578. doi: 10.2106/JBJS.H.00193
- Konishi, S., et al. “Risser sign and growth plate fusion as risk factors for scoliosis curve progression in adolescence.” Deformidade da coluna vertebral, vol. 7, no. 5, 2019, pp. 665-673. doi: 10.1016/j.jspd.2019.01.005
- Wagner, T., & Hardesty, C. K. “Recent advances in scoliosis screening and management.” Pediatric Annals, vol. 46, no. 10, 2017, pp. e381-e385. doi: 10.3928/19382359-20170921-01
- Negrini, S., et al. “Why the Risser sign remains important in scoliosis and how it can be enhanced for improved reliability.” Jornal Europeu da Coluna Vertebral, vol. 25, no. 2, 2016, pp. 263-267. doi: 10.1007/s00586-015-3866-y
- Dimeglio, A., & Canavese, F. “The growing spine: how spinal deformities influence normal spine and thoracic cage growth.” Jornal Europeu da Coluna Vertebral, vol. 21, no. 1, 2012, pp. 64-70. doi: 10.1007/s00586-011-1920-3
- Herring, J. A. “Tachdjian’s Pediatric Orthopaedics: From the Texas Scottish Rite Hospital for Children.” 5th ed., Elsevier, 2013.
- Soucacos, P. N., et al. “Predictors of scoliosis progression and bracing effectiveness in children with adolescent idiopathic scoliosis.” Jornal de Ortopedia Pediátrica, vol. 18, no. 6, 1998, pp. 741-745. doi: 10.1097/00004694-199811000-00006
- Bunnell, W. P. “The natural history of idiopathic scoliosis.” Ortopedia clínica e investigação relacionada, vol. 229, 1988, pp. 20-25. doi: 10.1097/00003086-198804000-00005
- Katz, D. E., et al. “Skeletal maturation of the hand and wrist: Evidence for a radiographic assessment method.” Jornal de Ortopedia Pediátrica, vol. 18, no. 6, 1998, pp. 742-747. doi: 10.1097/00004694-199811000-00007
- Vavruch, L., et al. “The predictive value of the Risser sign for scoliosis progression in adolescent idiopathic scoliosis.” Jornal Europeu da Coluna Vertebral, vol. 28, no. 4, 2019, pp. 904-910. doi: 10.1007/s00586-019-05943-9
- Lonstein, J. E. “Adolescent idiopathic scoliosis.” The Lancet, vol. 344, no. 8934, 1994, pp. 1407-1412. doi: 10.1016/S0140-6736(94)90540-1
- Weinstein, S. L., et al. “The Natural History of Adolescent Idiopathic Scoliosis.” Journal of Bone and Joint Surgery. American Volume, vol. 65, no. 4, 1983, pp. 447-455. doi: 10.2106/00004623-198365040-00012
- Scoliosis Research Society (SRS). “SRS Terminology and Measurements.” Sociedade de Investigação da Escoliose, 2021. Available at: www.srs.org
- Lou, E., et al. “Three-dimensional assessment of scoliosis correction by brace treatment using statistical shape modeling.” Deformidade da coluna vertebral, vol. 8, no. 5, 2020, pp. 929-935. doi: 10.1007/s43390-020-00128-9