Scoliosis and spondylosis are two distinct spinal conditions that can often coexist, leading to increased challenges in diagnosis and treatment. Scoliosis is a condition characterized by an abnormal curvature of the spine, while spondylosis refers to degenerative changes in the spine, such as osteoarthritis and disc degeneration. Both conditions can cause pain, limited mobility, and decreased quality of life. In this article, we will explore the relationship between scoliosis and spondylosis, discuss the diagnosis and assessment of these conditions, and explore various treatment options and integrative approaches for managing them.
The Relationship Between Scoliosis and Spondylosis
While scoliosis and spondylosis are distinct conditions, they often occur together, especially in older adults. Research suggests that the presence of scoliosis can increase the risk of developing spondylosis, and vice versa. The abnormal curvature of the spine in scoliosis can lead to uneven pressure on the spinal discs, accelerating degenerative changes. On the other hand, spondylosis can cause imbalances in the spine, leading to the development or progression of scoliosis. Understanding this relationship is crucial for effective management of both conditions.
Diagnosis and Assessment of Scoliosis and Spondylosis
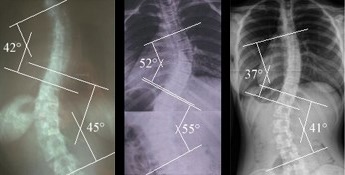
Accurate diagnosis and assessment of scoliosis and spondylosis are essential for developing an appropriate treatment plan. Diagnosis typically involves a thorough physical examination, including a visual assessment of the spine, measurement of the curvature using the Cobb angle, and imaging tests such as X-rays, MRI, or CT scans. Additionally, a detailed medical history and evaluation of symptoms are crucial for identifying the presence and severity of spondylosis. A multidisciplinary approach involving orthopedic specialists, radiologists, and physical therapists is often necessary to ensure an accurate diagnosis.
Conservative Treatment Options for Scoliosis and Spondylosis
Conservative treatment options are often the first line of management for scoliosis and spondylosis. These options aim to alleviate pain, improve mobility, and prevent further progression of the conditions. Physical therapy plays a crucial role in conservative treatment, focusing on strengthening the muscles surrounding the spine, improving posture, and increasing flexibility. Additionally, non-steroidal anti-inflammatory drugs (NSAIDs) and other pain medications may be prescribed to manage pain and inflammation associated with spondylosis.
Physical Therapy and Exercise for Managing Scoliosis and Spondylosis
Physical therapy and exercise are integral components of managing scoliosis and spondylosis. Specific exercises and stretches can help improve posture, strengthen the muscles supporting the spine, and increase flexibility. For scoliosis, exercises that focus on elongating the spine and correcting imbalances are often recommended. In spondylosis, exercises that improve joint mobility and strengthen the surrounding muscles can help alleviate pain and improve function. It is important to work with a qualified physical therapist who can tailor an exercise program to individual needs and monitor progress.

Bracing Techniques for Scoliosis and Spondylosis
Bracing is a common treatment option for scoliosis, especially in adolescents with moderate to severe curvature. Braces are designed to support the spine, prevent further progression of the curvature, and improve posture. Different types of braces are available, including the Boston brace, Milwaukee brace, and Charleston bending brace, each designed for specific types of scoliosis. In spondylosis, bracing may be used to provide stability and support to the affected area, reducing pain and improving function. However, bracing is typically not the primary treatment for spondylosis and is often used in conjunction with other therapies.
Surgical Interventions for Scoliosis and Spondylosis
In severe cases or when conservative treatments fail to provide relief, surgical interventions may be necessary for scoliosis and spondylosis. Spinal fusion is a common surgical procedure for scoliosis, where the vertebrae are fused together to correct the curvature. In spondylosis, surgical options may include decompression surgery to relieve pressure on nerves or spinal fusion to stabilize the affected area. These surgeries aim to reduce pain, improve function, and prevent further progression of the conditions. However, surgery is typically considered a last resort and is only recommended when the benefits outweigh the risks.
Integrative Approaches: Combining Traditional and Alternative Therapies
Integrative approaches that combine traditional medical treatments with alternative therapies can provide comprehensive care for individuals with scoliosis and spondylosis. These approaches recognize the importance of addressing physical, emotional, and psychological aspects of these conditions. Alternative therapies such as chiropractic care, acupuncture, massage therapy, and yoga can complement traditional treatments by promoting relaxation, reducing pain, and improving overall well-being. However, it is essential to consult with healthcare professionals and ensure the safety and effectiveness of these therapies.
Pain Management Strategies for Scoliosis and Spondylosis
Pain management is a crucial aspect of managing scoliosis and spondylosis. Chronic pain can significantly impact an individual’s quality of life and mental well-being. Non-pharmacological approaches such as heat or cold therapy, transcutaneous electrical nerve stimulation (TENS), and relaxation techniques can help alleviate pain. Additionally, medications such as analgesics, muscle relaxants, and nerve pain medications may be prescribed to manage pain associated with these conditions. It is important to work closely with healthcare professionals to develop an individualized pain management plan.
Psychological and Emotional Support for Individuals with Scoliosis and Spondylosis
Living with scoliosis and spondylosis can have a significant impact on an individual’s psychological and emotional well-being. Dealing with chronic pain, physical limitations, and body image concerns can lead to anxiety, depression, and decreased self-esteem. Therefore, providing psychological and emotional support is crucial in managing these conditions. Support groups, counseling, and cognitive-behavioral therapy can help individuals cope with the emotional challenges associated with scoliosis and spondylosis. It is important to address the holistic needs of individuals to achieve better outcomes.
Lifestyle Modifications for Managing Scoliosis and Spondylosis
In addition to medical treatments and therapies, lifestyle modifications can play a significant role in managing scoliosis and spondylosis. Maintaining a healthy weight, practicing good posture, avoiding heavy lifting or repetitive movements, and engaging in regular physical activity can help reduce the risk of further complications and improve overall well-being. Additionally, incorporating stress management techniques, such as mindfulness and relaxation exercises, can help individuals cope with the challenges of living with these conditions. It is important to work with healthcare professionals to develop a personalized lifestyle plan.
Future Directions: Advancements in Managing Scoliosis and Spondylosis
Advancements in medical technology and research continue to shape the management of scoliosis and spondylosis. Minimally invasive surgical techniques, such as endoscopic spine surgery, are being developed to reduce surgical risks and improve outcomes. Additionally, advancements in regenerative medicine, such as stem cell therapy, hold promise for repairing damaged spinal tissues and potentially reversing degenerative changes. Furthermore, the integration of artificial intelligence and machine learning algorithms in diagnostic and treatment planning processes may enhance accuracy and efficiency. Continued research and collaboration among healthcare professionals are essential for further advancements in managing scoliosis and spondylosis.
In conclusion, managing scoliosis and spondylosis together requires an integrated approach that addresses the unique challenges posed by these conditions. Accurate diagnosis, conservative treatments, physical therapy, bracing techniques, surgical interventions, integrative approaches, pain management strategies, psychological support, lifestyle modifications, and advancements in medical technology are all crucial components of comprehensive care. By combining traditional and alternative therapies, providing emotional support, and promoting healthy lifestyle habits, individuals with scoliosis and spondylosis can achieve better outcomes and improve their overall quality of life.
Referências
- Weinstein SL, Dolan LA, Wright JG, Dobbs MB. "Efeitos do aparelho em adolescentes com escoliose idiopática". Jornal de Medicina de Nova Inglaterra. 2013;369(16):1512-1521. doi: 10.1056/NEJMoa1307337.
- Schroeder GD, Kurd MF, Kepler CK, et al. “The management of cervical spondylotic myelopathy: current strategies, surgical outcomes, and controversies in the US.” O Jornal da Coluna Vertebral. 2018;18(2):216-225. doi: 10.1016/j.spinee.2017.09.008.
- Smith JS, Shaffrey CI, Berven S, et al. “Prospective multicenter assessment of risk factors for rod fracture following surgery for adult spinal deformity.” Jornal de Neurocirurgia: Coluna Vertebral. 2014;21(6):994-1003. doi: 10.3171/2014.8.SPINE131051.
- Katz JN, Harris MB. “Lumbar spinal stenosis.” Jornal de Medicina de Nova Inglaterra. 2008;358(8):818-825. doi: 10.1056/NEJMcp0708097.
- Weinstein JN, Lurie JD, Tosteson TD, et al. “Surgical versus nonoperative treatment for lumbar degenerative spondylolisthesis.” Jornal de Medicina de Nova Inglaterra. 2007;356(22):2257-2270. doi: 10.1056/NEJMoa070302.
- Shaffrey CI, Smith JS, Berven S, et al. “Defining pseudarthrosis in the setting of adult spinal deformity: a comprehensive review.” Lombada (Phila Pa 1976). 2013;38(22 Suppl 1). doi: 10.1097/BRS.0b013e3182a6a85a.
- O’Sullivan PB, Dankaerts W, O’Sullivan K, et al. “Multifactorial mechanisms in chronic low back pain: guidelines for management.” Terapia manual. 2012;17(4):267-275. doi: 10.1016/j.math.2012.03.002.
- Wright NC, Looker AC, Saag KG, et al. “The recent prevalence of osteoporosis and low bone mass in the United States based on bone mineral density at the femoral neck or lumbar spine.” Jornal de Investigação sobre Ossos e Minerais. 2014;29(11):2520-2526. doi: 10.1002/jbmr.2269.
- Fishman LM, Groessl EJ, Sherman KJ. “The use of yoga in managing chronic pain: A systematic review and meta-analysis.” Journal of Pain. 2017;18(12):1461-1472. doi: 10.1016/j.jpain.2017.07.008.
- Goh S, Price RI, Leedman PJ, et al. “Rehabilitation and outcome in idiopathic scoliosis following spinal fusion.” Revisões de fisioterapia. 2016;21(4-6):220-230. doi: 10.1080/10833196.2016.1251503.
- Berven SH, Lowe TG, Bradford DS. “The implications of deformity correction and instrumentation in the treatment of idiopathic scoliosis.” Volume americano do Journal of Bone and Joint Surgery. 2005;87(6):1224-1237. doi: 10.2106/JBJS.D.01731.
- Anjarwalla NK, Bhatia C, O’Neill KS. “Scoliosis correction and the effects on pulmonary function tests.” Jornal Bone & Joint. 2016;98-B(4):416-420. doi: 10.1302/0301-620X.98B4.36856.

