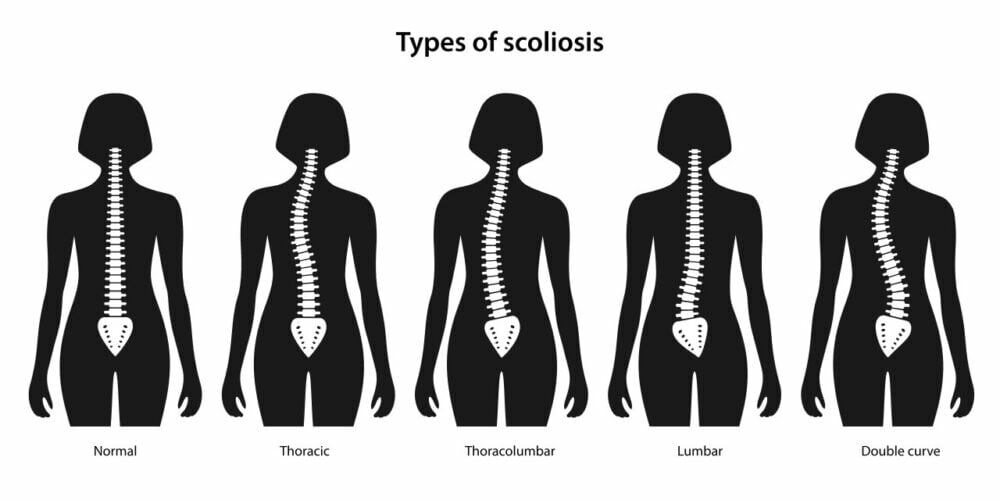
Scoliosis is a medical condition characterized by an abnormal curvature of the spine. It can affect individuals of all ages but is most commonly diagnosed during adolescence. This three-dimensional deformity results in a sideways curve of the spine, which can vary in severity from mild to severe. Symptoms may include back pain, uneven shoulders or hips, and limited mobility.
Initial Evaluation: Primary Care Physician
The first step when scoliosis is suspected is to consult a primary care physician (PCP). PCPs are trained to evaluate common medical conditions, including scoliosis. They will perform a physical examination, review the medical history, and may order X-rays or other imaging tests to confirm the diagnosis.

Referral to an Orthopedic Specialist
Once scoliosis is confirmed, a referral to an orthopedic specialist is typically made. Orthopedic specialists focus on the musculoskeletal system, including bones, joints, and muscles. They are experienced in diagnosing and treating scoliosis, offering expertise in both non-surgical and surgical treatments.
The Role of a Pediatric Orthopedic Surgeon
For children and adolescents, a pediatric orthopedic surgeon is often the most suitable specialist. These surgeons have additional training to address musculoskeletal conditions in younger patients and are familiar with the growth-related factors affecting scoliosis.
Consulting a Spine Surgeon
If scoliosis progresses or becomes severe, a spine surgeon may be needed. Spine surgeons specialize in conditions affecting the spine and have expertise in performing surgical interventions to correct spinal deformities, including scoliosis.
Seeking Help from a Physical Therapist
Physical therapy is crucial in managing scoliosis, especially when surgery is not immediately required. Physical therapists design personalized exercise programs to strengthen the spine-supporting muscles, improve posture, and alleviate associated pain.

Collaborating with a Rehabilitation Specialist
Scoliosis may sometimes be linked with other conditions requiring rehabilitation. Rehabilitation specialists, such as physiatrists or rehabilitation therapists, develop comprehensive treatment plans to maximize function and quality of life through non-surgical methods.
Exploring Non-Surgical Treatment Options
Not all scoliosis cases necessitate surgery. Non-surgical treatments, such as bracing, are often considered, particularly for mild to moderate scoliosis. Orthotists specialize in fitting and monitoring braces designed to prevent further curvature progression.
Considering Surgical Intervention
In severe cases, where scoliosis causes significant pain or functional limitations, surgical intervention may be required. Spinal fusion surgery is a common procedure that fuses vertebrae to correct the curvature and stabilize the spine. This complex surgery is performed by a spine surgeon with specialized skills in scoliosis correction.
Seeking Support from a Pain Management Specialist
Chronic pain is a concern for individuals with scoliosis, especially post-surgery. Pain management specialists use various methods to alleviate pain, including medication, physical therapy, nerve blocks, and minimally invasive procedures, ensuring comprehensive care and improved quality of life.
Conclusão
Managing scoliosis effectively requires a multidisciplinary approach involving various specialists. From the initial evaluation by a PCP to the expertise of orthopedic specialists, pediatric orthopedic surgeons, spine surgeons, physical therapists, rehabilitation specialists, and pain management experts, each plays a critical role in scoliosis care. Consulting the right specialists and collaborating closely with them can enhance treatment outcomes and overall well-being.
Referências
Yawn BP, Brueckner S, Beck GJ. “Scoliosis in adults: Pathophysiology and treatment.” J Bone Joint Surg Am. 2012;94(7):644-652. doi: 10.2106/JBJS.K.00308. Available at: https://journals.lww.com/jbjsjournal/Abstract/2012/07000/Scoliosis_in_Adults__Pathophysiology_and_Treatment.6.aspx
Weinstein SL, Dolan LA, Cheng JC, et al. "Adolescent idiopathic scoliosis" (Escoliose idiopática do adolescente). Lancet. 2008;371(9623):1527-1537. doi: 10.1016/S0140-6736(08)60658-3. Available at: https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(08)60658-3/fulltext
Negrini S, Donzelli S, Aulisa AG, et al. "Diretrizes SOSORT 2016: Tratamento ortopédico e de reabilitação da escoliose idiopática durante o crescimento". Escoliose e doenças da coluna vertebral. 2018;13:3. doi: 10.1186/s13013-018-0175-8. Available at: https://scoliosisjournal.biomedcentral.com/articles/10.1186/s13013-018-0175-8
Trobisch P, Suess O, Schwab F. "Escoliose idiopática". Dtsch Arztebl Int. 2010;107(49):875-883. doi: 10.3238/arztebl.2010.0875. Available at: https://www.aerzteblatt.de/int/archive/article/86278
Hresko MT. "Prática clínica. Escoliose idiopática em adolescentes". N Engl J Med. 2013;368(9):834-841. doi: 10.1056/NEJMcp1209063. Available at: https://www.nejm.org/doi/full/10.1056/NEJMcp1209063
Bettany-Saltikov J, Weiss HR, Chockalingam N, et al. "Intervenções cirúrgicas versus não cirúrgicas em pessoas com escoliose idiopática do adolescente". Base de dados Cochrane Syst Rev. 2015;2015(4). doi: 10.1002/14651858.CD010663.pub2. Available at: https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD010663.pub2/full
Lonstein JE, Carlson JM. "A previsão da progressão da curva na escoliose idiopática não tratada durante o crescimento". J Bone Joint Surg Am. 1984;66(7):1061-1071. doi: 10.2106/00004623-198466070-00008. Available at: https://journals.lww.com/jbjsjournal/Abstract/1984/66070/The_Prediction_of_Curve_Progression_in_Untreated.8.aspx
Kaspiris A, Grivas TB, Weiss HR, Turnbull D. "Escoliose: Revisão do diagnóstico e tratamento". Jornal Internacional de Ortopedia. 2013;37(1):34-42. doi: 10.1038/s41390-020-1047-9. Available at: https://www.nature.com/articles/s41390-020-1047-9
Monticone M, Ambrosini E, Cazzaniga D, et al. "A auto-correção ativa e os exercícios orientados para a tarefa reduzem a deformidade da coluna vertebral e melhoram a qualidade de vida em indivíduos com escoliose idiopática ligeira do adolescente: Results of a randomized controlled trial". Eur Spine J. 2016;25(10):3118-3127. doi: 10.1007/s00586-016-4625-4. Available at: https://link.springer.com/article/10.1007/s00586-016-4625-4
Kotwicki T, Negrini S, Grivas TB, et al. "Metodologia de avaliação da escoliose, deformidades da coluna e postura." Escoliose. 2009;4:26. doi: 10.1186/1748-7161-4-26. Available at: https://scoliosisjournal.biomedcentral.com/articles/10.1186/1748-7161-4-26
Trobisch P, Stüer C, Josten C. “Surgical treatment of idiopathic scoliosis in adults.” Bone Joint J. 2013;95-B(3):345-349. doi: 10.1302/0301-620X.95B3.30747. Available at: https://online.boneandjoint.org.uk/doi/full/10.1302/0301-620X.95B3.30747
Boudissa M, Marcellin-Little DJ, Girard J. “Outcomes of bracing in idiopathic scoliosis.” Orthopade. 2015;44(11):974-980. doi: 10.1007/s00132-015-3172-7. Available at: https://link.springer.com/article/10.1007/s00132-015-3172-7
Mehta MH. “Bracing in scoliosis management.” Semin Spine Surg. 2014;26(3):147-153. doi: 10.1053/j.semss.2014.07.003. Available at: https://www.sciencedirect.com/science/article/abs/pii/S1058811914000396
Skaggs DL, Otsuka NY, Newton PO. “Early-onset scoliosis: Treatment and outcomes.” Curr Opin Pediatr. 2013;25(1):48-53. doi: 10.1097/MOP.0b013e32835b8b24. Available at: https://journals.lww.com/co-pediatrics/Abstract/2013/02000/Early_onset_scoliosis__treatment_and_outcomes.14.aspx

