Scoliosis is a condition characterized by an abnormal curvature of the spine, which can lead to pain, discomfort, and even disability if left untreated. Early detection and intervention are crucial in managing scoliosis effectively. To ensure timely identification of this condition, various organizations and healthcare professionals have developed guidelines for scoliosis screening. These guidelines provide recommendations on who should be screened, how often screening should occur, and the methods and tools used for detection.

Understanding Scoliosis: Definition and Prevalence
Scoliosis is defined as a lateral curvature of the spine greater than 10 degrees, accompanied by rotation of the vertebrae. It can occur at any age, but it is most commonly diagnosed during adolescence. According to the Scoliosis Research Society, the prevalence of scoliosis ranges from 2% to 4% in the general population. It affects both males and females, although females are more likely to develop severe curves requiring treatment.
Importance of Early Detection: Why Scoliosis Screening Matters
Early detection of scoliosis is crucial because it allows for timely intervention and management. If left untreated, scoliosis can progress and lead to severe deformities, respiratory problems, and decreased quality of life. By identifying scoliosis early, healthcare providers can implement appropriate treatment plans, such as bracing or physical therapy, to prevent further progression of the curvature.
Age Groups for Scoliosis Screening: Who Should Be Screened?
The age at which scoliosis screening should begin varies among different guidelines. The American Academy of Orthopaedic Surgeons recommends screening for scoliosis in females at age 10 and in males at age 13. However, the Scoliosis Research Society suggests that screening should start at age 8 and continue until skeletal maturity. It is important to note that these guidelines are not universally agreed upon, and healthcare providers may have their own protocols based on individual patient risk factors.
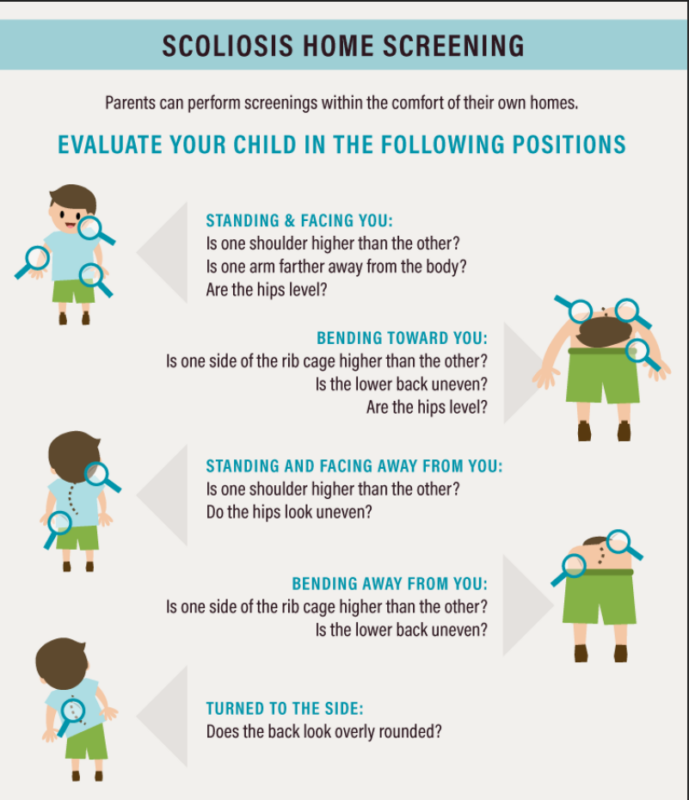
Screening Methods: Techniques and Tools Used for Scoliosis Detection
Scoliosis screening typically involves a physical examination, which includes assessing the patient’s posture, spinal alignment, and range of motion. The Adam’s Forward Bend Test is commonly used, where the patient bends forward at the waist while the healthcare provider observes for any asymmetry or abnormal curvature of the spine. In some cases, imaging tests such as X-rays or MRI scans may be necessary to confirm the diagnosis and assess the severity of the curvature.

Frequency of Screening: How Often Should Scoliosis Screening Occur?
The frequency of scoliosis screening depends on various factors, including the patient’s age, gender, and risk factors. The American Academy of Orthopaedic Surgeons recommends annual screening for adolescents until skeletal maturity. However, the Scoliosis Research Society suggests that screening should occur every 6 to 12 months during periods of rapid growth. It is important for healthcare providers to assess each patient individually and determine the appropriate screening frequency based on their specific needs.
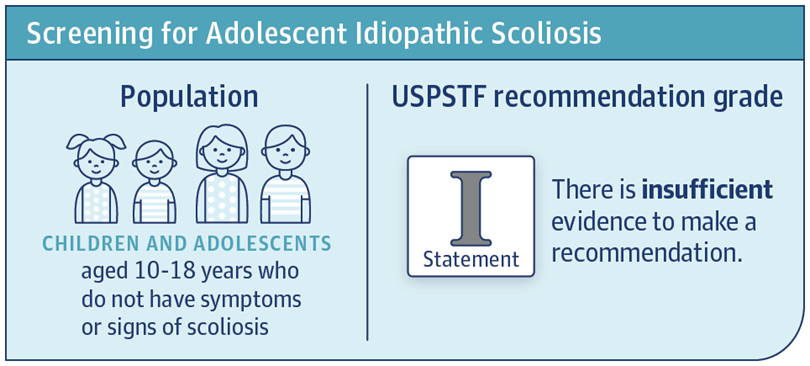
Key Recommendations: Latest Guidelines for Scoliosis Screening
The latest guidelines for scoliosis screening emphasize the importance of early detection and intervention. They recommend screening for scoliosis in adolescents, particularly females, starting at age 10 or 8, depending on the guideline. The guidelines also highlight the use of physical examination techniques, such as the Adam’s Forward Bend Test, as the primary screening method. Imaging tests are reserved for confirming the diagnosis and assessing the severity of the curvature.
Benefits and Limitations of Scoliosis Screening
Scoliosis screening offers several benefits, including early detection, timely intervention, and improved outcomes. By identifying scoliosis early, healthcare providers can implement appropriate treatment plans to prevent further progression of the curvature. However, scoliosis screening also has limitations. It may result in false positives, leading to unnecessary anxiety and additional testing. Additionally, not all cases of scoliosis can be detected through screening, especially in patients with mild or subtle curvature.
Role of Healthcare Providers: Who Should Conduct Scoliosis Screening?
Scoliosis screening can be conducted by various healthcare providers, including pediatricians, orthopedic surgeons, and school nurses. It is important for healthcare providers to have the necessary knowledge and skills to perform a thorough physical examination and interpret the findings accurately. Collaboration between healthcare providers and schools is also crucial in implementing scoliosis screening programs effectively.
Scoliosis Screening in Schools: Implementing Guidelines for Early Detection
Schools play a vital role in scoliosis screening, as they provide access to a large population of children and adolescents. Implementing guidelines for scoliosis screening in schools can help ensure early detection and intervention. School nurses can perform initial screenings using the Adam’s Forward Bend Test and refer students for further evaluation if necessary. Collaboration between schools, healthcare providers, and parents is essential in creating a comprehensive scoliosis screening program.

Treatment Options: What Happens After a Positive Scoliosis Screening?
After a positive scoliosis screening, further evaluation is necessary to confirm the diagnosis and assess the severity of the curvature. This may involve imaging tests, such as X-rays or MRI scans. Treatment options for scoliosis depend on the severity of the curvature and the patient’s age. Mild cases may only require monitoring, while more severe cases may require bracing or surgery. Physical therapy and exercises can also help improve posture and strengthen the muscles supporting the spine.
Conclusion: Promoting Awareness and Adherence to Scoliosis Screening Guidelines
Scoliosis screening guidelines are essential in promoting early detection and intervention for this condition. By adhering to these guidelines, healthcare providers can ensure that scoliosis is identified and managed effectively. Collaboration between healthcare providers, schools, and parents is crucial in implementing comprehensive scoliosis screening programs. By promoting awareness and adherence to these guidelines, we can improve outcomes for individuals with scoliosis and prevent the progression of this condition.
References
- Weinstein, S. L., Dolan, L. A., Cheng, J. C., et al. “Adolescent idiopathic scoliosis.” Lancet. 2008;371(9623):1527-1537. doi: 10.1016/S0140-6736(08)60658-3
- Negrini, S., Donzelli, S., Aulisa, A. G., et al. “2016 SOSORT guidelines: Orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth.” Scoliosis and Spinal Disorders. 2018;13:3. doi: 10.1186/s13013-018-0175-8
- Scoliosis Research Society. “Screening for scoliosis.” Available at: SRS Website
- American Academy of Orthopaedic Surgeons (AAOS). “Scoliosis in Children and Teens.” Available at: AAOS Website
- Bunnell, W. P. “Selectivity in screening for scoliosis.” Journal of Bone and Joint Surgery. 2005;87(9):1957-1962. doi: 10.2106/00004623-200509000-00001
- Lonstein, J. E., Carlson, J. M. “The prediction of curve progression in untreated idiopathic scoliosis during growth.” Journal of Bone and Joint Surgery. 1984;66(7):1061-1071. doi: 10.2106/00004623-198466070-00008
- Hresko, M. T. “Clinical practice. Idiopathic scoliosis in adolescents.” New England Journal of Medicine. 2013;368(9):834-841. doi: 10.1056/NEJMcp1209063
- Bettany-Saltikov, J., Weiss, H. R., Chockalingam, N., et al. “Surgical versus non-surgical interventions in people with adolescent idiopathic scoliosis.” Cochrane Database of Systematic Reviews. 2015;2015(4). doi: 10.1002/14651858.CD010663.pub2
- Richards, B. S., Vitale, M. G. “Screening for idiopathic scoliosis in adolescents: An information statement.” Journal of Bone and Joint Surgery. 2008;90(1):195-198. doi: 10.2106/JBJS.H.00452
- U.S. Preventive Services Task Force (USPSTF). “Screening for Adolescent Idiopathic Scoliosis: Recommendation Statement.” JAMA. 2018;319(2):165-172. doi: 10.1001/jama.2017.19342