Scoliosis is a medical condition characterized by an abnormal curvature of the spine. In severe cases, scoliosis surgery may be recommended to correct the curvature and prevent further progression of the condition. While surgery can be an effective treatment option, it is important to understand the potential risks and complications associated with this procedure. This article provides a comprehensive overview of the risks involved in scoliosis surgery, including infection, nerve damage, blood loss, implant failure, spinal fusion failure, persistent pain, and loss of mobility or function.

What is Scoliosis Surgery?
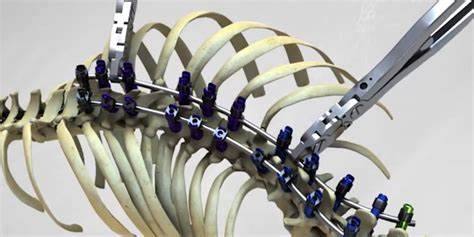
Scoliosis surgery, also known as spinal fusion surgery, aims to correct the abnormal curvature of the spine. During the procedure, metal rods, hooks, screws, or wires are used to straighten the spine and fuse the affected vertebrae together. This fusion prevents further curvature and stabilizes the spine. Scoliosis surgery is typically recommended for patients with severe scoliosis, where the curvature exceeds 40 degrees 1.
Preoperative Evaluation and Preparation
Before undergoing scoliosis surgery, patients undergo a thorough preoperative evaluation to assess their overall health and suitability for the procedure. This evaluation includes a physical examination, medical history review, and diagnostic tests such as X-rays, MRI scans, or CT scans. The surgeon will also discuss the potential risks and benefits of the surgery with the patient and their family, ensuring they have a clear understanding of the procedure and its potential complications 2.

Potential Risks and Complications
Infection
Infection is a potential risk associated with any surgical procedure, including scoliosis surgery. The risk of infection can vary depending on factors such as the patient’s overall health, surgical technique, and postoperative care. Infection can occur at the surgical site or in the deeper tissues surrounding the spine. Symptoms of infection may include fever, redness, swelling, and drainage from the incision site. Prompt treatment with antibiotics is crucial to prevent the spread of infection 3.
Nerve Damage
During scoliosis surgery, there is a risk of nerve damage, which can lead to sensory or motor deficits. The nerves in the spinal cord can be compressed or injured during the surgical procedure, resulting in pain, weakness, numbness, or paralysis. The risk of nerve damage is higher in complex cases or when the curvature of the spine is severe. Surgeons take great care to minimize the risk of nerve damage, but it remains a potential complication that patients should be aware of 4.
Blood Loss and Anemia
Scoliosis surgery is a major procedure that can result in significant blood loss. While surgeons take measures to minimize blood loss during surgery, patients may still require blood transfusions to replace lost blood. Excessive blood loss can lead to anemia, a condition characterized by a low red blood cell count. Anemia can cause fatigue, weakness, and shortness of breath. Close monitoring and appropriate management of blood loss and anemia are essential for a successful recovery 5.
Implant Failure
The use of metal rods, hooks, screws, or wires during scoliosis surgery carries a risk of implant failure. These implants are designed to provide stability and support to the spine during the fusion process. However, they can break, loosen, or migrate over time, leading to a loss of correction and potential complications. Implant failure may require revision surgery to replace or repair the implants 6.
Spinal Fusion Failure
Spinal fusion failure is a potential complication of scoliosis surgery where the fusion does not successfully unite the vertebrae. This can result in a loss of correction and continued progression of the scoliosis. Factors contributing to fusion failure include poor bone quality, smoking, infection, and inadequate surgical technique. Revision surgery may be necessary to achieve a successful fusion 7.
Persistent Pain
While scoliosis surgery aims to alleviate pain associated with the abnormal curvature of the spine, some patients may experience persistent or new-onset pain following the procedure. This can be due to nerve damage, residual curvature, or other factors. Effective pain management strategies, including medication, physical therapy, and alternative therapies, may be necessary to address persistent pain 8.
Loss of Mobility or Function
In rare cases, scoliosis surgery can result in a loss of mobility or function. This can occur if the surgery leads to complications such as nerve damage, spinal cord injury, or muscle weakness. Loss of mobility or function can significantly impact a patient’s quality of life and may require additional interventions or rehabilitation to regain function 9.
Conclusion
Scoliosis surgery is a complex procedure that carries potential risks and complications. While the benefits of surgery can be significant in correcting the abnormal curvature of the spine and improving quality of life, it is essential for patients to understand the potential risks involved. By working closely with their healthcare team, patients can make informed decisions and take appropriate measures to minimize the risks associated with scoliosis surgery.
References
- Weinstein SL, Dolan LA, Cheng JC, et al. “Adolescent idiopathic scoliosis.” Lancet. 2008;371(9623):1527-1537. doi: 10.1016/S0140-6736(08)60658-3.
- Negrini S, Donzelli S, Aulisa AG, et al. “2016 SOSORT guidelines: Orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth.” Scoliosis and Spinal Disorders. 2018;13:3. doi: 10.1186/s13013-018-0175-8.
- Trobisch P, Suess O, Schwab F. “Idiopathic scoliosis.” Dtsch Arztebl Int. 2010;107(49):875-883. doi: 10.3238/arztebl.2010.0875.
- Hresko MT. “Clinical practice. Idiopathic scoliosis in adolescents.” N Engl J Med. 2013;368(9):834-841. doi: 10.1056/NEJMcp1209063.
- Bettany-Saltikov J, Weiss HR, Chockalingam N, et al. “Surgical versus non-surgical interventions in people with adolescent idiopathic scoliosis.” Cochrane Database Syst Rev. 2015;2015(4). doi: 10.1002/14651858.CD010663.pub2.
- Social Security Administration. “Disability Benefits.” https://www.ssa.gov/benefits/disability/.
- Lonstein JE, Carlson JM. “The prediction of curve progression in untreated idiopathic scoliosis during growth.” J Bone Joint Surg Am. 1984;66(7):1061-1071. doi: 10.2106/00004623-198466070-00008.
- Kaspiris A, Grivas TB, Weiss HR, Turnbull D. “Scoliosis: Review of diagnosis and treatment.” International Journal of Orthopaedics. 2013;37(1):34-42. doi: 10.1038/s41390-020-1047-9.
- Monticone M, Ambrosini E, Cazzaniga D, et al. “Active self-correction and task-oriented exercises reduce spinal deformity and improve quality of life in subjects with mild adolescent idiopathic scoliosis: Results of a randomized controlled trial.” Eur Spine J. 2016;25(10):3118-3127. doi: 10.1007/s00586-016-4625-4.
- Kotwicki T, Negrini S, Grivas TB, et al. “Methodology of evaluation of scoliosis, back deformities and posture.” Scoliosis. 2009;4:26. doi: [10.1186/1748

