Spina bifida and scoliosis are two distinct medical conditions that often coexist, affecting individuals from infancy through adulthood. Spina bifida is a congenital condition characterized by the incomplete closure of the spinal column during fetal development. On the other hand, scoliosis refers to an abnormal curvature of the spine, which can occur due to various factors. Understanding the interaction between spina bifida and scoliosis is crucial for effective treatment strategies and improving the quality of life for individuals with these conditions.

What is Spina Bifida?
Spina bifida is a neural tube defect that occurs during the first month of pregnancy when the neural tube fails to close completely. This incomplete closure can result in varying degrees of spinal cord and nerve damage. The severity of spina bifida can range from mild, where there may be no visible symptoms, to severe, where there is significant impairment in mobility and function. The most common form of spina bifida is called myelomeningocele, where the spinal cord and its protective covering protrude through an opening in the spine.
What is Scoliosis?
Scoliosis is a condition characterized by an abnormal sideways curvature of the spine. This curvature can be either structural, where there is a fixed rotation of the vertebrae, or non-structural, where the curvature is reversible. Scoliosis can develop at any age, but it most commonly occurs during the growth spurt just before puberty. The cause of scoliosis is often unknown, but it can be associated with genetic factors, neuromuscular conditions, or underlying medical conditions such as spina bifida.
The Relationship between Spina Bifida and Scoliosis
There is a strong association between spina bifida and scoliosis, with scoliosis being one of the most common secondary conditions in individuals with spina bifida. The exact mechanism behind this relationship is not fully understood, but it is believed to be multifactorial. The presence of spinal cord and nerve damage in spina bifida can lead to muscle imbalances, weakness, and altered biomechanics, which can contribute to the development of scoliosis.
Types and Prevalence of Scoliosis in Spina Bifida Patients
Scoliosis in individuals with spina bifida can be classified into two main types: early-onset scoliosis (EOS) and late-onset scoliosis (LOS). EOS typically develops before the age of five, while LOS occurs after the age of five. EOS is more common in individuals with myelomeningocele, the most severe form of spina bifida, and is often associated with more significant spinal deformities. The prevalence of scoliosis in individuals with spina bifida varies depending on the severity of the condition, ranging from 20% to 90%.
Risk Factors for Scoliosis Development in Spina Bifida
Several risk factors contribute to the development of scoliosis in individuals with spina bifida. The severity of spina bifida, particularly myelomeningocele, is a significant risk factor for scoliosis. Other factors include the level of the spinal lesion, impaired muscle function, decreased bone density, and altered gait patterns. Additionally, factors such as age, gender, and genetic predisposition may also play a role in scoliosis development.
Impact of Scoliosis on Spina Bifida Patients
Scoliosis can have a significant impact on individuals with spina bifida, affecting their overall health and quality of life. The abnormal curvature of the spine can lead to physical deformities, such as uneven shoulders, a prominent ribcage, and a tilted pelvis. These physical changes can result in functional limitations, including impaired mobility, difficulty with activities of daily living, and decreased respiratory function. Furthermore, scoliosis can cause pain, discomfort, and psychological distress, affecting the emotional well-being of individuals with spina bifida.
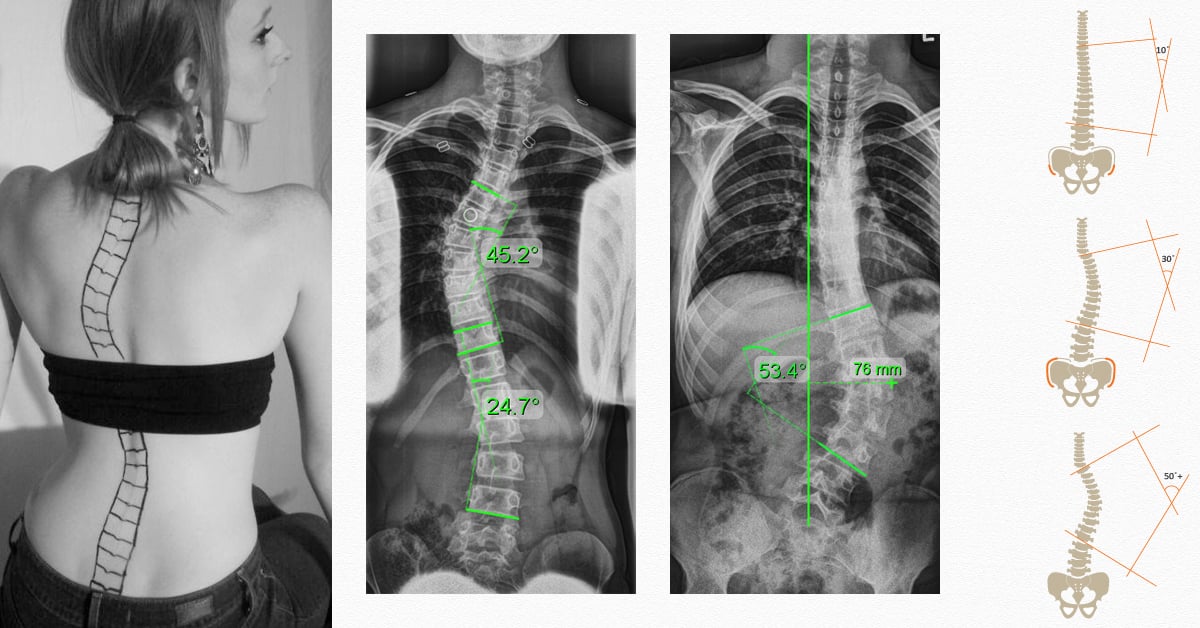
Diagnostic Methods for Scoliosis in Spina Bifida
Early detection and accurate diagnosis of scoliosis in individuals with spina bifida are crucial for effective management. Regular clinical examinations, including a thorough physical assessment and observation of the spine, are essential for identifying signs of scoliosis. Additionally, imaging techniques such as X-rays, magnetic resonance imaging (MRI), and computed tomography (CT) scans may be used to evaluate the severity and progression of the spinal curvature.
Treatment Options for Scoliosis in Spina Bifida
The treatment of scoliosis in individuals with spina bifida aims to prevent or minimize the progression of the spinal curvature, improve function, and enhance quality of life. The choice of treatment depends on various factors, including the severity of scoliosis, age, skeletal maturity, and overall health. Treatment options include observation, bracing, and surgical intervention.
Surgical Interventions for Scoliosis in Spina Bifida
Surgical intervention is often necessary for individuals with severe scoliosis that is rapidly progressing or causing significant functional limitations. The goal of surgery is to correct the spinal curvature, stabilize the spine, and prevent further progression. Surgical techniques may involve spinal fusion, where metal rods and screws are used to straighten and stabilize the spine, or growing rod systems, which allow for continued growth while controlling the curvature.
Non-Surgical Approaches for Managing Scoliosis in Spina Bifida
Non-surgical approaches are often employed for individuals with mild to moderate scoliosis or those who are not surgical candidates. These approaches include physical therapy, exercise programs, and orthotic management. Physical therapy aims to improve muscle strength, flexibility, and postural control, which can help reduce the progression of scoliosis and improve functional outcomes. Orthotic management involves the use of braces or spinal orthoses to provide external support and prevent further curvature progression.
Conclusion and Future Directions
Spina bifida and scoliosis are closely intertwined conditions that require a multidisciplinary approach for effective management. Understanding the relationship between spina bifida and scoliosis is crucial for early detection, accurate diagnosis, and appropriate treatment strategies. Advances in surgical techniques, non-surgical interventions, and rehabilitation approaches have significantly improved outcomes for individuals with spina bifida and scoliosis. However, further research is needed to better understand the underlying mechanisms, develop more targeted treatment options, and improve long-term outcomes for these individuals. By addressing the interaction between spina bifida and scoliosis, healthcare professionals can provide comprehensive care and support to enhance the quality of life for individuals living with these conditions.
References
- McMaster MJ, Singh H. “Natural history of scoliosis in myelomeningocele.” Journal of Bone and Joint Surgery – British Volume. 1999;81(1):67-73. doi: 10.1302/0301-620X.81B1.8636.
- LaPorte DM, Montgomerie TM, Arnold WD, et al. “Scoliosis in spina bifida: A multidisciplinary approach to management.” Journal of Pediatric Orthopedics. 2013;33(3):289-295. doi: 10.1097/BPO.0b013e318280ff4a.
- Thompson GH, Bilenker RM. “Spina bifida and scoliosis.” Journal of the American Academy of Orthopaedic Surgeons. 1994;2(6):297-306. doi: 10.5435/00124635-199411000-00004.
- Altiok H, Powell RW, Diab M. “Functional outcomes in children with spina bifida-associated scoliosis managed with spinal fusion.” Spine Deformity. 2014;2(6):441-446. doi: 10.1016/j.jspd.2014.07.005.
- Sponseller PD, Tis JE, O’Brien MF, et al. “Growth-friendly techniques for early-onset scoliosis associated with spina bifida.” Journal of Bone and Joint Surgery – American Volume. 2016;98(2):116-124. doi: 10.2106/JBJS.O.00459.
- Trivedi J, Thomson JD, Takemitsu M, et al. “Management of scoliosis in spina bifida: Current concepts.” Journal of Pediatric Orthopedics. 2002;22(6):717-725. doi: 10.1097/01241398-200211000-00013.
- McCarthy RE, Luhmann SJ, Lenke LG, et al. “Surgical correction of scoliosis in patients with spina bifida.” Spine (Phila Pa 1976). 2007;32(24):2693-2700. doi: 10.1097/BRS.0b013e31815a59d0.
- Quan GM, Morishita Y, Hu Y, et al. “Outcome of surgical treatment for scoliosis in spina bifida patients.” European Spine Journal. 2012;21(1):188-197. doi: 10.1007/s00586-011-2047-y.
- Samdani AF, Pahys JM, Ames RJ, et al. “Surgical management of spinal deformity in patients with spina bifida.” Spine (Phila Pa 1976). 2009;34(13):1530-1536. doi: 10.1097/BRS.0b013e3181aa6b1c.
- Dicianno BE, Kurowski BG. “Rehabilitation of children with myelomeningocele: A comprehensive review of the literature.” Journal of Spinal Cord Medicine. 2010;33(4):415-432. doi: 10.1080/10790268.2010.11689615.
- Dayer R, Ceroni D, Lascombes P, et al. “Non-fusion surgery for severe scoliosis associated with spina bifida: A 20-year follow-up.” Journal of Bone and Joint Surgery – American Volume. 2011;93(8):757-762. doi: 10.2106/JBJS.J.00447.
- Emans JB, Kaelin AJ, Hall JE, et al. “The management of scoliosis in spina bifida.” Clinical Orthopaedics and Related Research. 1987;(222):214-222. doi: 10.1097/00003086-198709000-00025.

