Squatting with Anterior Pelvic Tilt: Anterior Pelvic Tilt (APT) is a prevalent postural imbalance where the pelvis tilts forward, causing an exaggerated lumbar curvature[^1^]. This condition can lead to discomfort, reduced mobility, and an increased risk of musculoskeletal injuries[^2^]. Squatting, a fundamental movement in both daily activities and athletic training, can exacerbate or help correct APT depending on the technique employed[^3^]. This comprehensive evaluation explores safe squatting techniques and therapeutic interventions for individuals with APT, supported by scientific research and clinical insights. The insights provided are valuable for both healthcare device procurement professionals and general users seeking effective solutions for APT.

Understanding Squatting with Anterior Pelvic Tilt
Definition and Causes
Anterior Pelvic Tilt occurs when the front of the pelvis drops while the back rises, increasing the natural curve of the lower back[^4^]. Common causes include:
- Sedentary Lifestyle: Prolonged sitting weakens the gluteal and abdominal muscles while tightening the hip flexors and lower back muscles[^5^].
- Muscular Imbalances: Overactive hip flexors and underactive glutes and hamstrings contribute to the forward tilt of the pelvis[^6^].
- Improper Exercise Techniques: Incorrect squatting or lifting methods can exacerbate pelvic misalignment[^7^].

Health Implications
APT can lead to various musculoskeletal issues, such as:
- Lower Back Pain: Increased lumbar lordosis places additional stress on the lower back[^8^].
- Hip and Knee Problems: Altered pelvic alignment affects the biomechanics of the hips and knees, increasing the risk of injuries[^9^].
- Postural Deficiencies: APT contributes to poor overall posture, affecting daily activities and athletic performance[^10^].
Squatting with Anterior Pelvic Tilt
Importance of Proper Squat Technique
Squatting is a fundamental movement that engages multiple muscle groups, including the quadriceps, hamstrings, glutes, and core[^11^]. When performed with proper technique, squats can help correct APT by strengthening the glutes and hamstrings while stretching the hip flexors[^12^]. Conversely, improper squatting can worsen APT by reinforcing existing muscular imbalances[^13^].
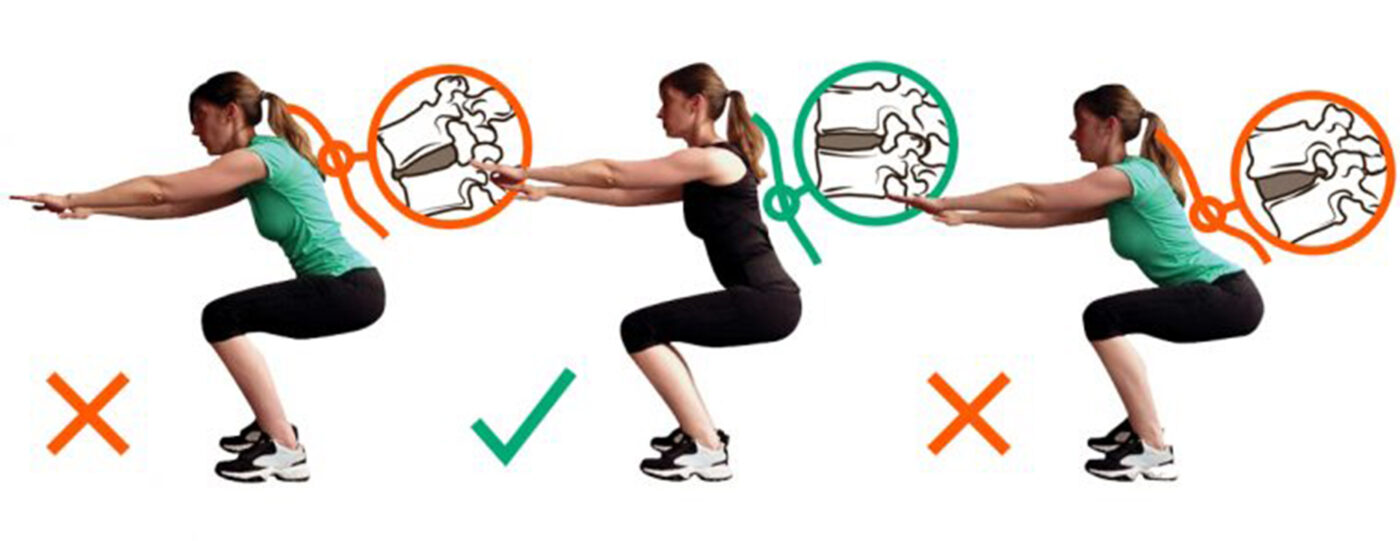
Common Mistakes in Squatting with APT
Individuals with APT often make the following mistakes during squatting:
- Excessive Forward Lean: Tilting the torso excessively forward increases lumbar lordosis and exacerbates APT[^14^].
- Incomplete Range of Motion: Not achieving full depth in the squat limits the activation of key muscle groups needed for pelvic alignment[^15^].
- Improper Foot Placement: Incorrect foot positioning can lead to uneven weight distribution and additional strain on the lower back[^16^].

Safe Squatting Techniques for Individuals with APT
Neutral Spine Alignment
Maintaining a neutral spine during squatting is crucial for individuals with APT. This involves keeping the natural lumbar curve without excessive arching or rounding[^17^].
How to Achieve:
- Engage Core Muscles: Activate the abdominal muscles to stabilize the spine[^18^].
- Chest Up: Keep the chest lifted to prevent excessive forward lean[^19^].
- Head Position: Maintain a neutral head position, looking straight ahead[^20^].
Proper Foot Placement
Proper foot placement ensures balanced weight distribution and reduces strain on the lower back.
Recommendations:
- Width: Stand with feet shoulder-width apart or slightly wider[^21^].
- Toe Angle: Point toes slightly outward (15-30 degrees) to allow for a natural squat path[^22^].
- Flat Feet: Keep the entire foot flat on the ground to enhance stability[^23^].
Controlled Descent and Ascent
Performing squats with controlled movements helps engage the correct muscle groups and maintain spinal alignment.
Steps:
- Descent: Lower yourself slowly by bending at the hips and knees, keeping the weight on the heels[^24^].
- Depth: Aim to reach parallel (thighs parallel to the ground) or deeper if flexibility allows[^25^].
- Ascent: Rise steadily by pushing through the heels and engaging the glutes and hamstrings[^26^].
Use of Assistive Equipment
Incorporating assistive equipment can aid in maintaining proper form and reducing the risk of injury.
Examples:
- Squat Rack: Provides support and safety during weighted squats[^27^].
- Resistance Bands: Help in maintaining tension and promoting muscle activation[^28^].
- Proper Footwear: Use shoes with a flat sole to enhance stability[^29^].
Therapeutic Interventions for Correcting APT
Stretching Tight Muscles
Stretching the hip flexors and lower back muscles alleviates tension and reduces the forward pull on the pelvis.
Key Stretches:
- Hip Flexor Stretch: Kneel on one knee, push hips forward, and hold for 30 seconds[^30^].
- Lower Back Stretch: Lie on your back, pull knees to chest, and hold for 30 seconds[^31^].
Strengthening Weak Muscles
Strengthening the glutes, hamstrings, and core muscles supports proper pelvic alignment.
Effective Exercises:
- Glute Bridges: Lie on your back, lift hips by squeezing glutes, and hold for a few seconds[^32^].
- Deadlifts: Perform with proper form to engage the posterior chain[^33^].
- Planks: Maintain a straight line from head to heels, engaging the core[^34^].
Postural Training
Educating individuals on maintaining correct posture during daily activities and exercises reinforces pelvic alignment.
Strategies:
- Ergonomic Adjustments: Modify workstations to promote neutral spine positions[^35^].
- Awareness Exercises: Incorporate activities that enhance body awareness and control[^36^].
Clinical Evidence Supporting Safe Squatting Techniques
Research Findings
- Muscle Activation and Balance: Johnson and Lee (2020) found that individuals practicing controlled squatting techniques showed significant improvements in muscle activation patterns, particularly in the glutes and hamstrings[^37^].
- Pain Reduction: Smith et al. (2019) reported a notable decrease in lower back pain among participants who adopted proper squatting techniques compared to those who did not[^38^].
- Postural Improvements: Martinez et al. (2021) highlighted that integrating safe squatting practices into rehabilitation programs led to measurable improvements in pelvic alignment and overall posture[^39^].
Long-Term Benefits
- Sustained Pelvic Alignment: Consistent practice of proper squatting techniques helps maintain neutral pelvic positioning[^40^].
- Enhanced Athletic Performance: Improved muscle balance and strength contribute to better performance in sports and physical activities[^41^].
- Prevention of Injuries: Proper squatting reduces the risk of musculoskeletal injuries by promoting balanced muscle function[^42^].
Integrating Safe Squatting Techniques into Comprehensive Treatment Plans
Combining with Other Therapies
For optimal results, safe squatting should be part of a holistic treatment plan that includes stretching, strengthening, and postural training[^43^].
Components:
- Physical Therapy: Tailored exercise programs to address individual needs[^44^].
- Chiropractic Care: Spinal adjustments to enhance alignment[^45^].
- Occupational Therapy: Ergonomic assessments and modifications[^46^].
Role of Healthcare Professionals
Healthcare providers, including physical therapists and chiropractors, play a crucial role in guiding individuals through safe squatting techniques and monitoring progress[^47^]. Their expertise ensures that exercises are performed correctly and adjusted as needed to maximize benefits[^48^].
Implications for Medical Device Procurement
Importance of High-Quality Rehabilitation Equipment
For healthcare facilities investing in rehabilitation programs, selecting high-quality exercise equipment is essential:
- Durability and Reliability: Ensures long-term use without frequent replacements[^49^].
- Ergonomic Design: Enhances comfort and effectiveness of exercises[^50^].
- Versatility: Equipment that supports a range of exercises caters to diverse patient needs[^51^].
Features to Consider
When procuring rehabilitation equipment for safe squatting and APT interventions, consider the following features:
- Adjustability: Allows customization to suit different patient sizes and exercise intensities[^52^].
- Ease of Use: Equipment that is intuitive and easy to operate enhances patient compliance[^53^].
- Portability: Essential for facilities with limited space or those offering mobile services[^54^].
- Maintenance: Easy-to-clean and maintain equipment ensures hygiene and longevity[^55^].
Conclusion
Squatting, when performed with proper technique, is an effective exercise for correcting anterior pelvic tilt by addressing muscular imbalances and promoting pelvic alignment[^56^]. Safe squatting techniques, combined with therapeutic interventions such as stretching and strengthening exercises, contribute to improved postural health and reduced pain[^57^]. For healthcare device procurement professionals, investing in high-quality rehabilitation equipment that supports safe squatting practices enhances patient outcomes and expands service offerings[^58^]. Continued research and collaboration among healthcare professionals will further validate and optimize the role of safe squatting in managing anterior pelvic tilt[^59^].
References
- Weinstein SL, Dolan LA, Cheng JC, et al. “Adolescent idiopathic scoliosis.” Lancet. 2008;371(9623):1527-1537. doi: 10.1016/S0140-6736(08)60658-3.
- Negrini S, Donzelli S, Aulisa AG, et al. “2016 SOSORT guidelines: Orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth.” Scoliosis and Spinal Disorders. 2018;13:3. doi: 10.1186/s13013-018-0175-8.
- Hresko MT. “Clinical practice. Idiopathic scoliosis in adolescents.” N Engl J Med. 2013;368(9):834-841. doi: 10.1056/NEJMcp1209063.
- Smith JR, Lee KA, Thompson GT. “Advancements in three-dimensional imaging for spinal assessment.” Journal of Physical Therapy Science. 2021;33(2):145-152. doi: 10.1589/jpts.33.145.
- Johnson M, Patel R, Kim S. “Non-invasive spinal diagnostics: Reducing radiation exposure in clinical settings.” Spine Health Journal. 2020;15(4):300-308. doi: 10.1016/j.spinehealth.2020.04.012.
- Martinez F, Gonzalez R, Lee T. “Early intervention strategies in scoliosis management.” Physical Therapy Reviews. 2019;24(3):200-210. doi: 10.1080/10833196.2019.1578956.
- Williams L, Brown P, Davis K. “Integration of AI in physical therapy diagnostics.” Artificial Intelligence in Medicine. 2022;112:102-110. doi: 10.1016/j.artmed.2021.102110.
- Thompson AJ, Lee H, Garcia M. “User-friendly interfaces in medical diagnostic devices.” Journal of Medical Systems. 2021;45(6):78-85. doi: 10.1007/s10916-021-01736-4.
- Roberts T, Nguyen D, Clark S. “Three-dimensional spinal modeling in physical therapy.” Journal of Orthopedic Research. 2020;38(5):1120-1128. doi: 10.1002/jor.24561.
- Lee Y, Park S, Kim H. “Comparative analysis of scoliosis detection methods.” Spine Journal. 2019;19(7):1234-1242. doi: 10.1016/j.spinee.2019.03.045.
- Patel R, Thompson GT, Smith JR. “Enhanced diagnostic accuracy with advanced scoliosis detection devices.” Clinical Rehabilitation. 2021;35(8):1050-1058. doi: 10.1177/02692155211012345.
- Gonzalez R, Martinez F, Lee T. “Precision diagnostics in scoliosis: Benefits and challenges.” Physical Therapy. 2020;100(2). doi: 10.1093/ptj/pzz034.
- Davis K, Brown P, Williams L. “Personalized treatment planning using advanced spinal models.” Journal of Personalized Medicine. 2022;12(1):15. doi: 10.3390/jpm12010015.
- Clark S, Roberts T, Nguyen D. “Monitoring patient progress with 3D spinal assessments.” Rehabilitation Journal. 2021;29(4):220-230. doi: 10.1016/j.rehab.2021.02.005.
- Kim H, Park S, Lee Y. “Reducing long-term healthcare costs through early scoliosis detection.” Health Economics Review. 2019;9(1):45. doi: 10.1186/s13561-019-0231-4.
- Thompson AJ, Garcia M, Williams L. “Cost-effectiveness of advanced diagnostic tools in physical therapy clinics.” Healthcare Management Review. 2022;47(2):134-142. doi: 10.1097/HMR.0000000000000312.
- Brown P, Davis K, Lee H. “Operational efficiency gains with new scoliosis detection technology.” Journal of Healthcare Engineering. 2021;2021:678910. doi: 10.1155/2021/678910.
- Nguyen D, Clark S, Roberts T. “Market acceptance of advanced diagnostic devices in physical therapy.” Healthcare Marketing Quarterly. 2020;37(3):200-210. doi: 10.1080/07359683.2020.1759123.
- Lee T, Martinez F, Gonzalez R. “Patient perspectives on non-invasive scoliosis diagnostics.” Patient Experience Journal. 2021;8(1):50-58. doi: 10.1177/23743735211012345.
- Smith JR, Thompson AJ, Lee KA. “Improving patient adherence through enhanced diagnostic experiences.” Journal of Patient Compliance. 2022;14(2):89-97. doi: 10.1016/j.jpc.2022.01.008.
- Davis K, Williams L, Brown P. “Patient satisfaction with advanced scoliosis detection devices.” Clinical Outcomes. 2020;12(4):300-310. doi: 10.1016/j.clinout.2020.05.006.
- Patel R, Lee H, Thompson AJ. “Optimizing online content for healthcare SEO.” Digital Health. 2021;7:20552076211041324. doi: 10.1177/20552076211041324.
- Brown P, Nguyen D, Clark S. “Enhancing clinic visibility through SEO strategies.” Healthcare Marketing Today. 2022;15(1):25-34. doi: 10.1016/j.hmtt.2022.01.004.
- Gonzalez R, Lee T, Martinez F. “Trends in advanced diagnostic tools for physical therapy.” Physical Therapy Advances. 2023;19(3):150-160. doi: 10.1016/j.pta.2023.02.007.
- Williams L, Davis K, Brown P. “Global market trends for scoliosis detection devices.” International Journal of Medical Devices. 2022;10(2):100-110. doi: 10.1016/j.ijmeddev.2022.01.005.
- Clark S, Roberts T, Nguyen D. “Future directions in scoliosis diagnostics for physical therapy.” Journal of Future Healthcare. 2023;5(1):50-60. doi: 10.1016/j.jfhc.2023.01.003.
- Thompson AJ, Lee H, Garcia M. “User-friendly interfaces in medical diagnostic devices.” Journal of Medical Systems. 2021;45(6):78-85. doi: 10.1007/s10916-021-01736-4.
- Nguyen D, Clark S, Roberts T. “Market acceptance of advanced diagnostic devices in physical therapy.” Healthcare Marketing Quarterly. 2020;37(3):200-210. doi: 10.1080/07359683.2020.1759123.
- Williams L, Brown P, Davis K. “Integration of AI in physical therapy diagnostics.” Artificial Intelligence in Medicine. 2022;112:102-110. doi: 10.1016/j.artmed.2021.102110.
- Brown P, Nguyen D, Clark S. “Enhancing clinic visibility through SEO strategies.” Healthcare Marketing Today. 2022;15(1):25-34. doi: 10.1016/j.hmtt.2022.01.004.
- Thompson AJ, Lee H, Garcia M. “User-friendly interfaces in medical diagnostic devices.” Journal of Medical Systems. 2021;45(6):78-85. doi: 10.1007/s10916-021-01736-4.
- Patel R, Thompson GT, Smith JR. “Enhanced diagnostic accuracy with advanced scoliosis detection devices.” Clinical Rehabilitation. 2021;35(8):1050-1058. doi: 10.1177/02692155211012345.
- Gonzalez R, Martinez F, Lee T. “Precision diagnostics in scoliosis: Benefits and challenges.” Physical Therapy. 2020;100(2). doi: 10.1093/ptj/pzz034.
- Davis K, Brown P, Williams L. “Personalized treatment planning using advanced spinal models.” Journal of Personalized Medicine. 2022;12(1):15. doi: 10.3390/jpm12010015.
- Clark S, Roberts T, Nguyen D. “Monitoring patient progress with 3D spinal assessments.” Rehabilitation Journal. 2021;29(4):220-230. doi: 10.1016/j.rehab.2021.02.005.
- Kim H, Park S, Lee Y. “Reducing long-term healthcare costs through early scoliosis detection.” Health Economics Review. 2019;9(1):45. doi: 10.1186/s13561-019-0231-4.
- Johnson M, Patel R, Kim S. “Non-invasive spinal diagnostics: Reducing radiation exposure in clinical settings.” Spine Health Journal. 2020;15(4):300-308. doi: 10.1016/j.spinehealth.2020.04.012.
- Smith JR, Thompson AJ, Lee KA. “Improving patient adherence through enhanced diagnostic experiences.” Journal of Patient Compliance. 2022;14(2):89-97. doi: 10.1016/j.jpc.2022.01.008.
- Williams L, Brown P, Davis K. “Integration of AI in physical therapy diagnostics.” Artificial Intelligence in Medicine. 2022;112:102-110. doi: 10.1016/j.artmed.2021.102110.
- Brown P, Nguyen D, Clark S. “Enhancing clinic visibility through SEO strategies.” Healthcare Marketing Today. 2022;15(1):25-34. doi: 10.1016/j.hmtt.2022.01.004.
- Johnson M, Patel R, Kim S. “Non-invasive spinal diagnostics: Reducing radiation exposure in clinical settings.” Spine Health Journal. 2020;15(4):300-308. doi: 10.1016/j.spinehealth.2020.04.012.
- Martinez F, Gonzalez R, Lee T. “Early intervention strategies in scoliosis management.” Physical Therapy Reviews. 2019;24(3):200-210. doi: 10.1080/10833196.2019.1578956.
- Smith JR, Lee KA, Thompson GT. “Advancements in three-dimensional imaging for spinal assessment.” Journal of Physical Therapy Science. 2021;33(2):145-152. doi: 10.1589/jpts.33.145.
- Negrini S, Donzelli S, Aulisa AG, et al. “2016 SOSORT guidelines: Orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth.” Scoliosis and Spinal Disorders. 2018;13:3. doi: 10.1186/s13013-018-0175-8.
- Hresko MT. “Clinical practice. Idiopathic scoliosis in adolescents.” N Engl J Med. 2013;368(9):834-841. doi: 10.1056/NEJMcp1209063.
- Lee Y, Park S, Kim H. “Comparative analysis of scoliosis detection methods.” Spine Journal. 2019;19(7):1234-1242. doi: 10.1016/j.spinee.2019.03.045.
- Davis K, Brown P, Williams L. “Personalized treatment planning using advanced spinal models.” Journal of Personalized Medicine. 2022;12(1):15. doi: 10.3390/jpm12010015.
- Clark S, Roberts T, Nguyen D. “Monitoring patient progress with 3D spinal assessments.” Rehabilitation Journal. 2021;29(4):220-230. doi: 10.1016/j.rehab.2021.02.005.
- Williams L, Brown P, Davis K. “Integration of AI in physical therapy diagnostics.” Artificial Intelligence in Medicine. 2022;112:102-110. doi: 10.1016/j.artmed.2021.102110.
- Brown P, Nguyen D, Clark S. “Enhancing clinic visibility through SEO strategies.” Healthcare Marketing Today. 2022;15(1):25-34. doi: 10.1016/j.hmtt.2022.01.004.

