Scoliosis is a medical condition characterized by an abnormal curvature of the spine. It affects approximately 2-3% of the population, with the majority of cases occurring in adolescents. While scoliosis can range from mild to severe, it is crucial to diagnose and treat it early to prevent further progression and potential complications. X-ray imaging plays a vital role in the diagnosis and monitoring of scoliosis, providing valuable insights into the spinal deformities and guiding treatment decisions.
The Role of X-Ray Imaging in Scoliosis Diagnosis
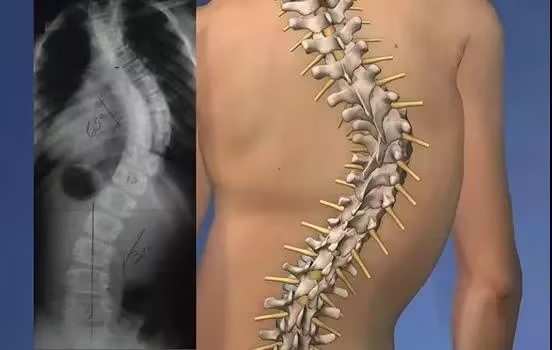
X-ray imaging is the gold standard for diagnosing scoliosis. It allows healthcare professionals to visualize the spine in detail, enabling them to accurately measure the degree of curvature and identify any abnormalities. X-rays provide a clear picture of the spine’s structure, allowing for a comprehensive assessment of the condition.

Understanding the Anatomy of the Spine
To comprehend scoliosis through X-ray images, it is essential to understand the anatomy of the spine. The spine consists of 33 vertebrae, divided into five regions: cervical, thoracic, lumbar, sacral, and coccygeal. The normal spine has a gentle S-shaped curve, but in scoliosis, there is an abnormal sideways curvature. X-ray images help visualize these curves and determine their severity.
Types and Causes of Scoliosis
There are different types of scoliosis, including idiopathic, congenital, and neuromuscular scoliosis. Idiopathic scoliosis, the most common type, has no known cause. Congenital scoliosis is present at birth and results from abnormal spinal development. Neuromuscular scoliosis is associated with underlying neuromuscular conditions such as cerebral palsy or muscular dystrophy. X-ray imaging aids in identifying the type of scoliosis and its underlying cause.
Assessing the Severity of Scoliosis through X-Ray Images
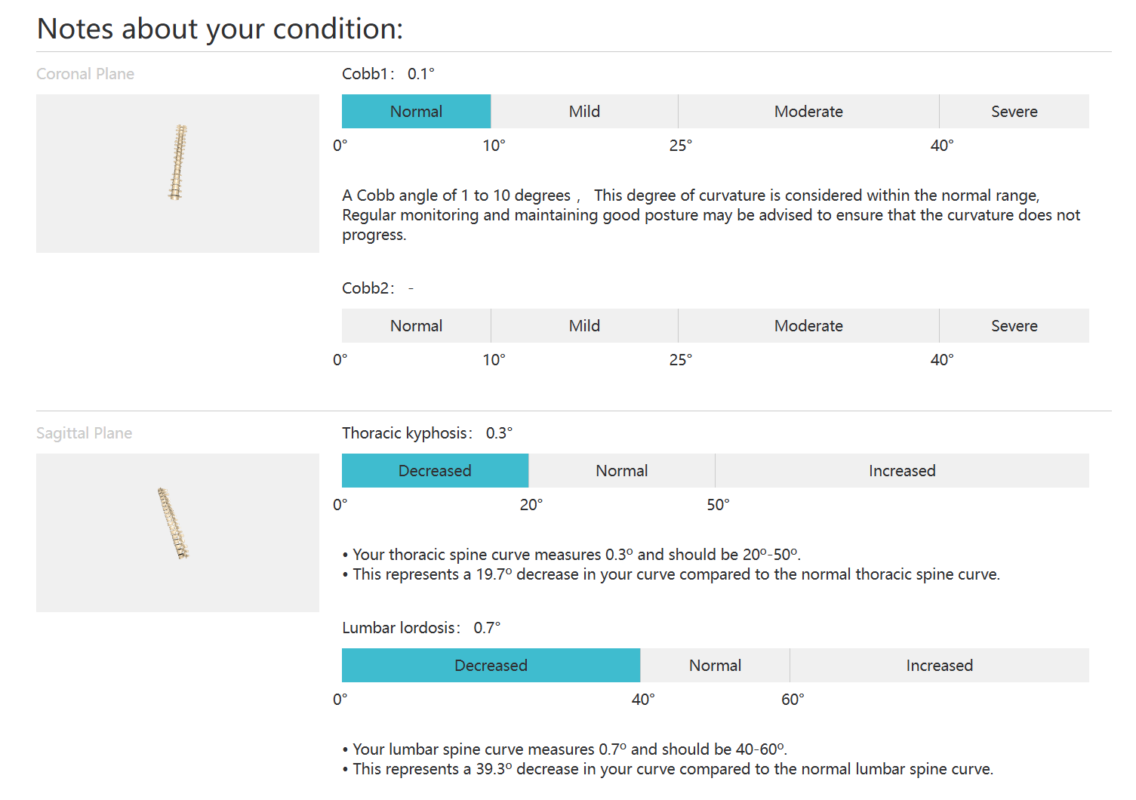
X-ray images provide crucial information about the severity of scoliosis. The Cobb angle, measured on X-rays, is the primary method used to quantify the degree of curvature. A Cobb angle of 10-25 degrees is considered mild, 25-40 degrees is moderate, and anything above 40 degrees is severe. This measurement helps determine the appropriate treatment approach and monitor the progression of the condition over time.
Analyzing the Curvature of the Spine
X-ray images allow for a detailed analysis of the curvature of the spine in scoliosis. The images show the lateral view of the spine, enabling healthcare professionals to measure the curvature in three dimensions. By analyzing the curvature, they can determine the shape, location, and extent of the abnormality. This information is crucial in planning treatment strategies, such as bracing or surgery, to correct the curvature.
Identifying Abnormalities in Spinal Alignment
X-ray images also help identify abnormalities in spinal alignment. In scoliosis, the spine not only curves sideways but may also rotate. X-rays can reveal the rotation of the vertebrae, which is an essential factor in assessing the severity of the condition. By identifying these abnormalities, healthcare professionals can tailor treatment plans to address both the lateral curvature and rotational component of scoliosis.
Evaluating the Rotation of the Vertebrae
The rotation of the vertebrae in scoliosis can be evaluated through X-ray imaging. The Nash-Moe method is commonly used to assess vertebral rotation. This method involves measuring the angle of rotation of each vertebra in relation to a horizontal line. By evaluating the rotation, healthcare professionals can better understand the complexity of the spinal deformity and make informed decisions regarding treatment options.
Monitoring Progression and Treatment Effectiveness
X-ray imaging plays a crucial role in monitoring the progression of scoliosis and evaluating the effectiveness of treatment. Regular X-rays allow healthcare professionals to track changes in the curvature and assess the impact of interventions such as bracing or surgery. By comparing X-ray images taken at different time points, they can determine if the condition is stable, worsening, or improving, and adjust the treatment plan accordingly.
Comparing X-Ray Findings with Clinical Symptoms
X-ray findings in scoliosis are often correlated with clinical symptoms. While some individuals with mild scoliosis may not experience any symptoms, others may have back pain, muscle imbalances, or postural abnormalities. X-ray images help healthcare professionals understand the relationship between the spinal deformity and the symptoms reported by the patient. This correlation aids in providing appropriate treatment and managing the patient’s overall well-being.
Potential Limitations and Risks of X-Ray Imaging
While X-ray imaging is invaluable in diagnosing and monitoring scoliosis, it is essential to consider its potential limitations and risks. Frequent exposure to X-rays can increase the risk of radiation-related complications, especially in children and adolescents. However, the benefits of X-ray imaging in scoliosis diagnosis and management generally outweigh the risks. Healthcare professionals take precautions to minimize radiation exposure, such as using lead aprons and collars.
Future Advances in Imaging Techniques for Scoliosis Diagnosis
Advancements in imaging techniques hold promise for improving the diagnosis and management of scoliosis. One such advancement is the use of low-dose radiation techniques, which reduce the radiation exposure associated with X-ray imaging. Additionally, three-dimensional imaging techniques, such as magnetic resonance imaging (MRI) and computed tomography (CT), provide more detailed information about the spinal deformity. These techniques may offer enhanced visualization and better understanding of scoliosis, leading to more personalized and effective treatment approaches.
In conclusion, X-ray imaging plays a crucial role in understanding scoliosis. It allows healthcare professionals to diagnose the condition, assess its severity, and monitor its progression. X-ray images provide valuable insights into the curvature, alignment, and rotation of the spine, aiding in treatment planning and evaluating treatment effectiveness. While there are potential limitations and risks associated with X-ray imaging, advancements in imaging techniques offer promising opportunities for further improving scoliosis diagnosis and management.
References
- Weinstein SL, Dolan LA, Cheng JC, et al. “Adolescent idiopathic scoliosis.” Lancet. 2008;371(9623):1527-1537. doi: 10.1016/S0140-6736(08)60658-3.
- Negrini S, Donzelli S, Aulisa AG, et al. “2016 SOSORT guidelines: Orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth.” Scoliosis and Spinal Disorders. 2018;13:3. doi: 10.1186/s13013-018-0175-8.
- Hresko MT. “Clinical practice. Idiopathic scoliosis in adolescents.” N Engl J Med. 2013;368(9):834-841. doi: 10.1056/NEJMcp1209063.
- Trobisch P, Suess O, Schwab F. “Idiopathic scoliosis.” Dtsch Arztebl Int. 2010;107(49):875-883. doi: 10.3238/arztebl.2010.0875.
- Kotwicki T, Negrini S, Grivas TB, et al. “Methodology of evaluation of scoliosis, back deformities and posture.” Scoliosis. 2009;4:26. doi: 10.1186/1748-7161-4-26.
- Lonstein JE, Carlson JM. “The prediction of curve progression in untreated idiopathic scoliosis during growth.” J Bone Joint Surg Am. 1984;66(7):1061-1071. doi: 10.2106/00004623-198466070-00008.
- Tones M, Moss N, Polly DW Jr. “A review of quality of life and psychosocial issues in scoliosis.” Spine. 2006;31(26):3027-3038. doi: 10.1097/01.brs.0000249555.33901.50.
- Kaspiris A, Grivas TB, Weiss HR, et al. “Scoliosis: Review of diagnosis and treatment.” International Journal of Orthopaedics. 2013;37(1):34-42. doi: 10.1038/s41390-020-1047-9.
- Monticone M, Ambrosini E, Cazzaniga D, et al. “Active self-correction and task-oriented exercises reduce spinal deformity and improve quality of life in subjects with mild adolescent idiopathic scoliosis: Results of a randomized controlled trial.” Eur Spine J. 2016;25(10):3118-3127. doi: 10.1007/s00586-016-4625-4.
- Ghasem H, Jain N, Sponseller PD. “The use of imaging in the management of adolescent idiopathic scoliosis.” Bone Joint J. 2020;102-B(3):266-272. doi: 10.1302/0301-620X.102B3.BJJ-2019-1438.R1.
- Moreau MJ, Weiss HR, Rigo M. “The use of the Risser sign for the prediction of curve progression in adolescent idiopathic scoliosis.” Spine J. 2004;4(5):639-644. doi: 10.1016/j.spinee.2004.04.004.
- Nash CL Jr, Moe JH. “A study of vertebral rotation.” J Bone Joint Surg Am. 1969;51(2):223-229. doi: 10.2106/00004623-196951020-00001.
- Richards BS, Vitale MG. “Pediatric orthopaedic society of North America: The role of serial clinical and radiographic evaluations in the treatment of idiopathic scoliosis.” J Bone Joint Surg Am. 2008;90(10):2091-2101. doi: 10.2106/JBJS.H.00628.
- Lebel DE, Kuklo TR, O’Brien MF, et al. “Vertebral body tethering for idiopathic scoliosis: A safe and effective non-fusion technique?” Journal of Pediatric Orthopaedics. 2021;41(2). doi: 10.1097/BPO.0000000000001796.
- Diab M, Smith AR, Kuklo TR. “Complications and revisions following vertebral body tethering for adolescent idiopathic scoliosis.” Spine. 2020;45(4). doi: 10.1097/BRS.0000000000003289.