Idiopathic scoliosis is a complex spinal condition that manifests as an abnormal curvature of the spine, primarily affecting adolescents during their growth years. The assessment of idiopathic scoliosis is a multifaceted process that involves a combination of clinical examinations, imaging studies, and, in some cases, advanced technological tools. We will delve into the intricacies of idiopathic scoliosis assessment, exploring the key components, diagnostic criteria, available imaging modalities, and emerging technologies that contribute to a thorough evaluation of this enigmatic condition in this comprehensive guide.
Understanding Idiopathic Scoliosis
Definition and Characteristics:
Idiopathic scoliosis is a three-dimensional deformity of the spine characterized by a lateral curvature that typically emerges during adolescence. The term “idiopathic” denotes that the exact cause of the condition is unknown, differentiating it from scoliosis with identifiable causes such as congenital factors or neuromuscular disorders.
The hallmark of idiopathic scoliosis is an abnormal curvature when viewed from the front or back, resembling an ‘S’ or ‘C’ shape. While the majority of cases are mild and do not cause significant health issues, severe forms can lead to complications such as chronic back pain and respiratory problems.
Clinical Idiopathic Scoliosis Assessment
Physical Examination:
Clinical assessment begins with a thorough physical examination conducted by a healthcare professional, often a pediatrician, orthopedic surgeon, or spine specialist. Key components of the physical examination include:
Forward Bend Test (Adam’s Test):
The patient bends forward at the waist, allowing the examiner to observe any asymmetry or prominence of the spine.
This test helps identify potential signs of scoliosis, such as rib hump or uneven shoulder blades.
Shoulder Height and Pelvic Alignment:
Assessment of shoulder height and pelvic alignment aids in detecting any noticeable asymmetry that may indicate spinal curvature.
Gait and Posture:
Observing the patient’s gait and overall posture provides additional insights into the presence of scoliosis.
Neurological Examination:
A neurological examination may be conducted to assess reflexes, muscle strength, and sensation, ruling out secondary causes of scoliosis.
Diagnostic criteria of idiopathic scoliosis assessment
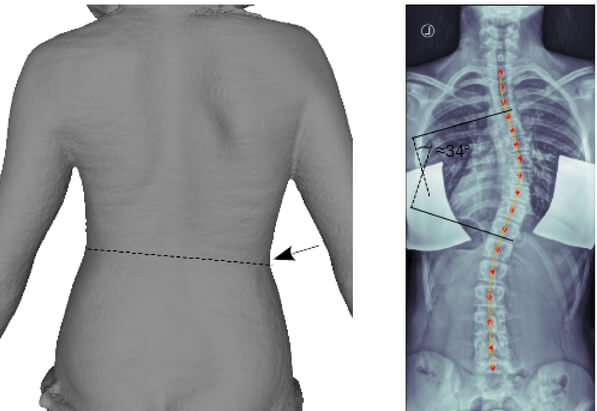
To quantify the degree of spinal curvature and determine the severity of scoliosis, the Cobb angle measurement is employed. This measurement is derived from X-ray images and involves:
1. Identification of End Vertebrae: The most tilted vertebrae at the top and bottom of the curvature are identified.
2. Perpendicular Lines and Angle Measurement: Perpendicular lines are drawn from the superior endplate of the upper end vertebra and the inferior endplate of the lower end vertebra.
The angle formed at the intersection of these lines is the Cobb angle, expressed in degrees.
- Classification of Severity:
Based on the Cobb angle measurement, idiopathic scoliosis is classified into three categories:
1. Mild Scoliosis: Cobb angle between 10 and 25 degrees.
2. Moderate Scoliosis: Cobb angle ranging from 25 to 40 degrees.
3. Severe Scoliosis: Cobb angle exceeding 40 degrees.
The classification helps guide treatment decisions and interventions.
Imaging Modalities of idiopathic scoliosis assessment
X-rays:
X-rays remain a fundamental imaging modality in idiopathic scoliosis assessment. They provide detailed images of the spine in both frontal and lateral planes, enabling precise measurement of the Cobb angle and visualization of the spinal curvature.
Magnetic Resonance Imaging (MRI):
While less commonly used for routine scoliosis assessment, MRI may be employed in specific cases to assess spinal cord and nerve root integrity. It is particularly useful when evaluating for other potential causes of spinal curvature or when surgery is being considered.
Computed Tomography (CT) Scan:
CT scans offer detailed cross-sectional images of the spine, providing additional information about the bony structures. They are more commonly used when surgical intervention is planned, allowing for precise preoperative planning.
Emerging technologies in idiopathic scoliosis assessment
In the ever-evolving landscape of medical technology, innovations that challenge traditional approaches often pave the way for more efficient and patient-friendly solutions. Forethought’s Handheld Screening for Scoliosis is a prime example of such innovation, heralding a new era in the assessment of spinal deformities. This handheld device not only eliminates the need for X-rays but incorporates advanced features like Smart Light Sensing Technology and Accurate Terrain Scanning, making scoliosis assessments more accessible and precise than ever before.
Beyond Traditional Radiography:
The traditional approach to scoliosis assessment typically involves X-rays, which, while effective, come with inherent drawbacks such as radiation exposure. Forethought’s Handheld Screening for Scoliosis challenges this norm by introducing a non-radiometric method that prioritizes patient safety without compromising diagnostic accuracy. Forethought’s Handheld Screening for Scoliosis represents a transformative step in the field of spinal assessment. By incorporating Smart Light Sensing Technology, Accurate Terrain Scanning, and 3D reporting, this innovative device not only enhances the precision of scoliosis evaluations but also makes the entire process more patient-friendly and accessible.
1. Smart Light Sensing Technology:
At the core of Forethought’s innovation is its Smart Light Sensing Technology, a groundbreaking feature that dynamically captures small angular velocity changes using MEMS (Micro-Electro-Mechanical Systems) sensors. This technology allows for the precise measurement of spinal curvature without the need for traditional radiographic methods.
The MEMS sensors, known for their sensitivity and accuracy, enable real-time data acquisition by detecting even the slightest shifts in the spine. This not only enhances the diagnostic capabilities of the device but also minimizes the discomfort associated with conventional imaging methods.
2. Accurate Terrain Scanning Technology:
Forethought’s Handheld Screening for Scoliosis goes beyond spinal curvature measurement; it introduces Accurate Terrain Scanning Technology, a feature designed to adapt to the speed and movements of the operator. This ensures the collection of the most reliable terrain data, offering a more holistic view of the spinal landscape.
a. Operator-Speed Adaptive Scanning:
The device intelligently adjusts its scanning parameters based on the speed and movements of the operator. This adaptive scanning feature ensures that the data collected accurately represents the nuances of the patient’s spinal structure.
b. Multi-Level, Multi-Space Information:
Accurate Terrain Scanning Technology doesn’t stop at individualized scanning; it incorporates multi-level, multi-space information for complementary and optimal combination processing. This approach ensures that the data collected from different perspectives is seamlessly integrated, providing a comprehensive understanding of the spinal terrain.
3D Reporting for Diagnostic Assistance:
A major leap forward in Forethought’s Handheld Screening for Scoliosis is its utilization of 3D reporting for diagnostic assistance. This feature transforms raw data into a three-dimensional representation of the spinal curvature, offering healthcare professionals a more detailed and nuanced view of the deformity.
1. Enhanced Visualization:
The 3D reporting not only aids in accurate diagnosis but also enhances the visualization of the scoliotic curves. This allows healthcare professionals to assess the severity and complexity of the condition more comprehensively, leading to more informed treatment decisions.
2. Patient Engagement:
Moreover, the 3D representation can be a valuable tool for patient engagement. Patients can visually grasp the nature of their spinal condition, fostering better communication and understanding between healthcare providers and those undergoing scoliosis assessments.
3. Making Assessments More Accessible:
The paradigm shift introduced by Forethought’s Handheld Screening for Scoliosis is not confined to technological advancements alone. It addresses a crucial aspect of accessibility, especially in settings where traditional radiographic equipment may not be readily available.
4. Portable and User-Friendly Design:
The handheld nature of the device enhances its portability, making scoliosis assessments possible in diverse healthcare settings. Its user-friendly design empowers healthcare professionals to conduct screenings efficiently, providing timely assessments in environments ranging from clinics to community outreach programs.
5. Pediatric and Adolescent Health:
This accessibility is particularly significant in the realm of pediatric and adolescent health. Children and adolescents, being more susceptible to the effects of radiation, benefit from a non-radiometric approach that ensures accurate assessments without unnecessary exposure.
Psychosocial Assessment
Beyond the physical aspects, idiopathic scoliosis assessment should also consider the psychosocial impact on the individual, especially adolescents. The visible changes in body appearance may contribute to self-esteem issues, and healthcare professionals should be attuned to the emotional well-being of those affected.
Treatment Decision-Making
The culmination of the assessment process leads to treatment decision-making. The approach to idiopathic scoliosis management depends on factors such as the severity of the curvature, skeletal maturity, and the potential for progression. Treatment options range from observation for mild cases to bracing and, in severe cases, surgical intervention.
In navigating the complex terrain of idiopathic scoliosis assessment, a comprehensive approach that combines clinical examination, precise measurements, and advanced imaging technologies is essential. The Cobb angle measurement remains a cornerstone in evaluating the severity of spinal curvature, while emerging technologies, such as 3D imaging and innovative handheld devices, contribute to a more holistic understanding of the condition. As we continue to refine our methods and embrace cutting-edge technologies, the goal remains steadfast—to provide accurate assessments that guide personalized treatment plans, ensuring the optimal management of idiopathic scoliosis and enhancing the quality of life for those affected.
References
- Hresko MT. “Clinical Practice: Idiopathic Scoliosis in Adolescents.” New England Journal of Medicine. 2013;368(9):834-841. doi: 10.1056/NEJMcp1209063.
- Weinstein SL, Dolan LA, Wright JG, Dobbs MB. “Effects of Bracing in Adolescents with Idiopathic Scoliosis.” New England Journal of Medicine. 2013;369(16):1512-1521. doi: 10.1056/NEJMoa1307337.
- Sanders JO, Newton PO, Browne RH, et al. “Bracing for Idiopathic Scoliosis: How Many Patients Require Treatment to Prevent One Surgery?” Journal of Bone and Joint Surgery American Volume. 2014;96(8):649-653. doi: 10.2106/JBJS.M.00329.
- Schreiber S, Parent EC, Hedden DM, et al. “The Effect of Schroth Exercises Added to the Standard of Care on the Quality of Life and Muscle Endurance in Adolescents with Idiopathic Scoliosis: An Assessor and Statistician Blinded Randomized Controlled Trial.” BMC Musculoskeletal Disorders. 2015;16(1):263. doi: 10.1186/s12891-015-0689-8.
- Maruyama T, Takeshita K, Kitagawa T. “Conservative Treatment for Adolescent Idiopathic Scoliosis: Can It Reduce the Incidence of Surgical Treatment?” Pediatric Rehabilitation. 2003;6(3-4):215-219. doi: 10.1080/13638490310001636793.
- Misterska E, Glowacki M, Latuszewska J. “Patient and Parental Assessment of Appearance in Adolescent Idiopathic Scoliosis Treated with a Brace: A Case-Control Study.” Journal of Pediatric Orthopaedics B. 2013;22(1):26-33. doi: 10.1097/BPB.0b013e3283599ee1.
- Cobb JR. “Outline for the Study of Scoliosis.” Instructional Course Lectures. 1948;5:261-275.
- Tsirikos AI, Sud A. “Current Concepts and Controversies in the Surgical Management of Adolescent Idiopathic Scoliosis.” Bone & Joint Journal. 2012;94(12):1541-1552. doi: 10.1302/0301-620X.94B12.30270.
- Goldberg CJ, Moore DP, Fogarty EE, Dowling FE. “Adolescent Idiopathic Scoliosis: The Effect of Brace Treatment on the Incidence of Surgery.” Spine. 2001;26(1):42-47. doi: 10.1097/00007632-200101010-00009.
- Forethought Medical. “Innovative Scoliosis Screening and Management Solutions.” Forethought Medical Technology, 2023.
- Weiss HR, Moramarco M. “Scoliosis—Treatment Indications According to Current Evidence.” Current Pediatric Reviews. 2013;9(1):55-59. doi: 10.2174/1573396311309010009.
- Sucato DJ, “Management of Adolescent Idiopathic Scoliosis.” Orthopedic Clinics of North America. 2007;38(4):469-478. doi: 10.1016/j.ocl.2007.07.002.
- Nash CL Jr., Moe JH. “A Study of Vertebral Rotation.” Journal of Bone and Joint Surgery American Volume. 1969;51(2):223-229. doi: 10.2106/00004623-196951020-00004.
- Mac-Thiong JM, Labelle H. “Advances in Imaging and Assessing Spinal Deformities.” Journal of Pediatric Orthopaedics. 2012;32(1). doi: 10.1097/BPO.0b013e31823a11f3.
- Bunnell WP. “Selective Screening for Scoliosis.” Clinical Orthopaedics and Related Research. 2005;434:40-45. doi: 10.1097/01.blo.0000161249.07309.bf.

