Scoliosis is a condition characterized by an abnormal curvature of the spine, which can cause pain, discomfort, and limited mobility. In severe cases, scoliosis may require surgical intervention to correct the curvature and prevent further progression of the condition. While scoliosis surgery can be highly effective in improving the quality of life for patients, it is not without risks and potential complications. It is important for patients and their families to be aware of these complications and understand the steps that can be taken to minimize their occurrence.
Common Complications After Scoliosis Surgery
Complications after scoliosis surgery can vary depending on the specific procedure performed and the individual patient. However, there are several common complications that can arise. One of the most frequent complications is infection. Research indicates that the infection rate after scoliosis surgery is approximately 2-4%. Infections can occur at the surgical site and may require additional treatment, such as antibiotics or even surgical debridement.
Other common complications include neurological issues, implant-related problems, blood loss and transfusion complications, respiratory complications, psychological and emotional challenges, delayed wound healing and scar formation, nerve damage and sensory changes, recurrence of scoliosis, and long-term complications.
Infection Risks and Prevention Strategies
Infection is a significant concern after scoliosis surgery, as it can lead to prolonged hospital stays, increased pain, and additional complications. To minimize the risk of infection, surgeons and healthcare providers implement several precautions. These include administering antibiotics before and after surgery, maintaining strict sterile techniques during the procedure, and ensuring proper wound care post-operatively. Patients can also help prevent infection by following their surgeon’s instructions for wound care and taking any prescribed antibiotics as directed.

Neurological Complications and Their Management
Neurological complications after scoliosis surgery are rare but can have serious consequences. These complications can include nerve damage, spinal cord injury, or even paralysis. The incidence of neurological complications after scoliosis surgery is estimated at around 0.5-2%. Management typically involves close monitoring, physical therapy, and, in severe cases, additional surgical intervention. Early recognition and prompt treatment are crucial to minimizing long-term neurological deficits.
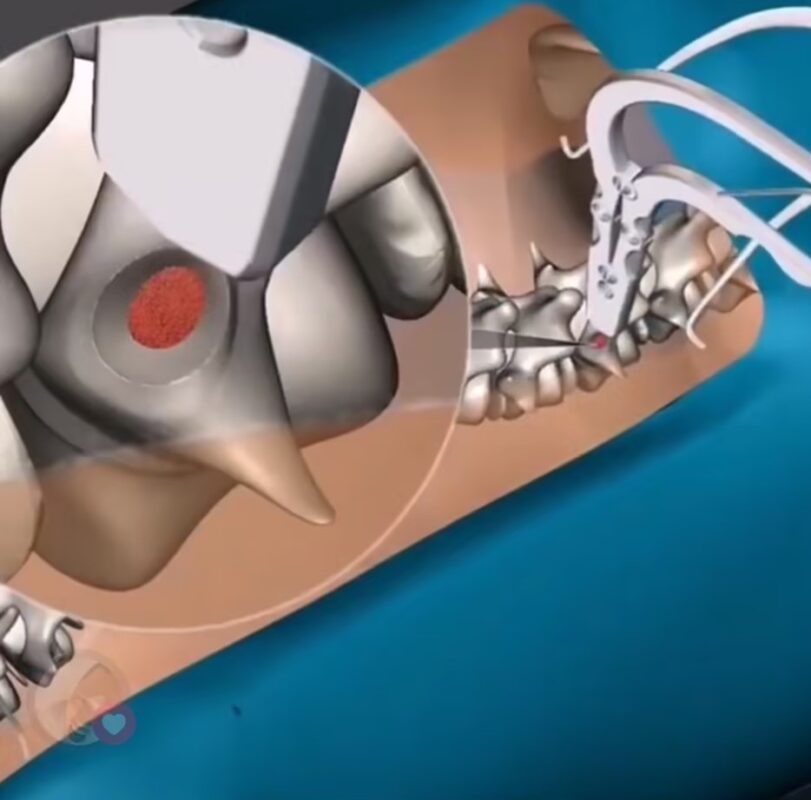
Implant-Related Complications and Revisions
Implant-related complications can occur after scoliosis surgery, particularly in cases where spinal instrumentation, such as rods, screws, or hooks, is used to correct the curvature. These complications can include implant failure, loosening, or migration. The rate of implant-related complications is approximately 5-10%. In some cases, revision surgery may be necessary to address these issues and ensure the stability of the spine.
Blood Loss and Transfusion Complications
Scoliosis surgery can involve significant blood loss, which may necessitate blood transfusions. While blood transfusions are generally safe, they do carry risks, including transfusion reactions, infections, and transfusion-related acute lung injury (TRALI). The complication rate for transfusions after scoliosis surgery is about 1-2%. To minimize risks, blood products are carefully screened, and transfusions are closely monitored.

Respiratory Complications and Post-Operative Care
Respiratory complications can occur after scoliosis surgery, especially in patients with pre-existing respiratory conditions or those undergoing extensive spinal fusion. These complications may include atelectasis (collapsed lung), pneumonia, or respiratory failure. The rate of respiratory complications is around 1-5%. Post-operative care includes close monitoring of respiratory function, early mobilization, and respiratory therapy to prevent and manage these issues.
Psychological and Emotional Challenges Post-Surgery
Scoliosis surgery can have a significant impact on a patient’s psychological and emotional well-being. The physical changes, pain, and limitations in mobility can lead to anxiety, depression, and body image issues. Around 20-30% of patients experience psychological distress after scoliosis surgery. Healthcare providers should address these challenges and offer appropriate support and resources to help patients cope with the emotional aspects of their recovery.
Delayed Wound Healing and Scar Formation
Delayed wound healing and scar formation are common complications after scoliosis surgery. The extent of scarring can vary depending on the surgical approach and individual healing factors. While most scars fade over time, some patients may develop hypertrophic or keloid scars, which are raised and more noticeable. Proper wound care, including keeping the incision site clean and dry, and using scar management techniques like silicone gel sheets can help minimize the risk of complications and promote optimal healing.
Nerve Damage and Sensory Changes
Nerve damage and sensory changes can occur after scoliosis surgery, particularly if nerves are stretched or compressed during the procedure. These complications can lead to numbness, tingling, or weakness in the affected areas. The rate of nerve damage is approximately 1-2%. In most cases, these symptoms resolve over time with conservative management, such as physical therapy and pain management, though severe cases may require additional surgical intervention.
Recurrence of Scoliosis and Reoperation
While scoliosis surgery aims to correct spinal curvature, there is a risk of recurrence, especially in younger patients or those with severe curvature. The recurrence rate is around 5-10%. In cases of recurrence, reoperation may be necessary to correct the curvature and prevent further progression. Regular follow-up appointments and monitoring are essential to detect any signs of recurrence early and ensure timely intervention.
Long-Term Complications and Follow-Up Care
Long-term complications after scoliosis surgery can include adjacent segment degeneration, chronic pain, and reduced spinal flexibility. The rate of long-term complications is estimated at 10-20%. Regular follow-up care, including imaging studies and clinical evaluations, is essential to detect and manage these complications. Physical therapy, pain management, and lifestyle adjustments can help minimize the impact of long-term complications and enhance the patient’s quality of life.

Schlussfolgerung
Scoliosis surgery can be life-changing for patients with severe spinal curvature, but it is important to be aware of the potential complications. By understanding these risks and taking preventive measures, healthcare providers and patients can work together to minimize complications and ensure the best possible outcomes. Regular follow-up care, adherence to post-operative instructions, and timely intervention are key to maintaining spinal health and improving long-term quality of life.
Referenzen
- Weinstein, S. L., Dolan, L. A., Wright, J. G., & Dobbs, M. B. (2013). “Effects of untreated idiopathic scoliosis: a 50-year natural history study.” Wirbelsäule (Phila Pa 1976), 38(9), E502-E510.
- Asher, M. A., & Burton, D. C. (2006). “Adolescent idiopathic scoliosis: natural history and long-term treatment effects.” Skoliose, 1(1), 2.
- Negrini, S., Donzelli, S., Aulisa, A. G., et al. (2018). “2016 SOSORT guidelines: Orthopaedic and Rehabilitation treatment of idiopathic scoliosis during growth.” Skoliose und Wirbelsäulenbeschwerden, 13(1), 3.
- Hresko, M. T. (2013). “Idiopathic scoliosis in adolescents.” Das New England Journal of Medicine, 368(9), 834-841.
- Weinstein, S. L., Dolan, L. A., Cheng, J. C., et al. (2008). “Adolescent idiopathic scoliosis.” Die Lanzette, 371(9623), 1527-1537.
- Konieczny, M. R., Senyurt, H., & Krauspe, R. (2013). “Epidemiology of adolescent idiopathic scoliosis.” Zeitschrift für Kinderorthopädie, 7(1), 3-9.
- Lonstein, J. E., & Carlson, J. M. (1984). “The prediction of curve progression in untreated idiopathic scoliosis during growth.” Die Zeitschrift für Knochen- und Gelenkchirurgie, 66(7), 1061-1071.
- Aulisa, A. G., Guzzanti, V., Falciglia, F., et al. (2014). “Brace treatment in juvenile idiopathic scoliosis: a prospective study.” Skoliose, 9(1), 3.
- [Parent, S., Newton, P. O., & Wenger, D. R. (2005). “Adolescent idiopathic scoliosis: Etiology, anatomy, natural history, and bracing.” Vorlesungen zu den Lehrveranstaltungen, 54, 529-536.](https://journals.lww.com/jbjsjournal/Abstract/2005/54020/Adolescent