La escoliosis es una enfermedad caracterizada por una curvatura anormal de la columna vertebral. Afecta a millones de personas en todo el mundo, con distintos grados de gravedad. Tradicionalmente, la escoliosis se ha tratado con corsés ortopédicos o cirugía de fusión espinal. Sin embargo, los avances de la tecnología médica han llevado al desarrollo de un procedimiento de vanguardia conocido como anclaje de la escoliosis. El objetivo de este artículo es ofrecer una visión general de la fijación de la columna vertebral para la escoliosis, incluido su procedimiento, ventajas, riesgos, criterios de elegibilidad, recuperación, resultados a largo plazo y comparación con otras opciones quirúrgicas.
Comprender la escoliosis: Causas y síntomas
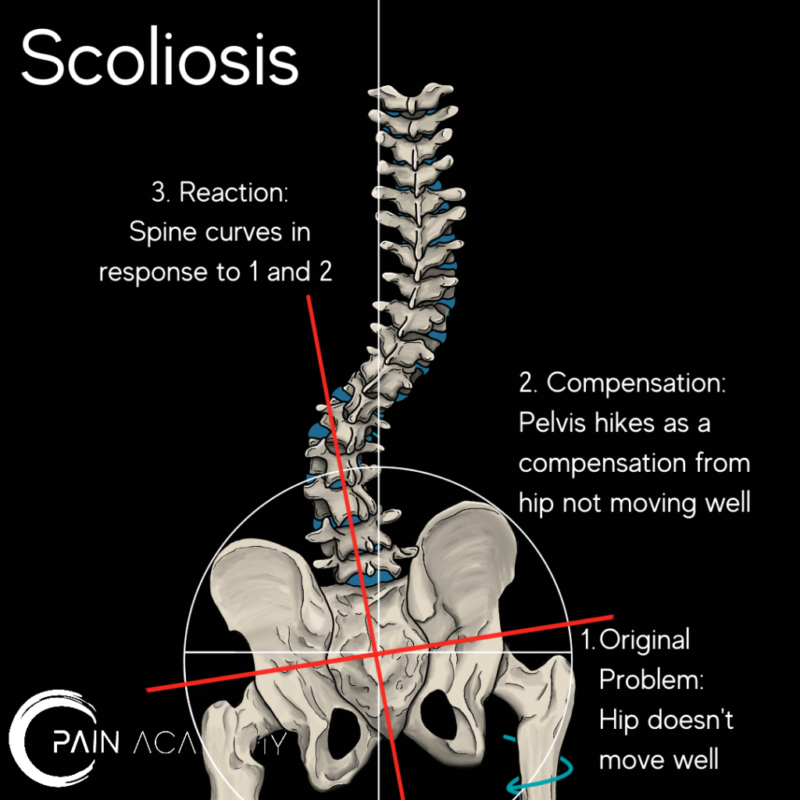
Antes de profundizar en la escoliosis atada, es esencial comprender las causas y los síntomas de la escoliosis. La escoliosis puede clasificarse como idiopática, lo que significa que se desconoce la causa, o no idiopática, que puede estar causada por factores como afecciones neuromusculares, anomalías congénitas o traumatismos. La forma más común de escoliosis es la idiopática, que suele aparecer durante la adolescencia.
Los síntomas de la escoliosis pueden variar en función de la gravedad de la curvatura. Los casos leves pueden mostrar sólo una ligera asimetría en los hombros o las caderas, mientras que los casos más graves pueden causar deformidades notables de la columna vertebral, como una joroba o una prominencia costal. Además, la escoliosis puede provocar dolor de espalda, movilidad limitada y problemas respiratorios en los casos graves.
Tratamientos tradicionales de la escoliosis
Históricamente, la escoliosis se ha tratado con corsés o cirugía de fusión espinal. Los corsés suelen recomendarse a los pacientes con escoliosis moderada para evitar que la curvatura siga progresando. Sin embargo, los corsés no siempre son eficaces para corregir la curvatura y pueden resultar incómodos y restrictivos para el paciente.
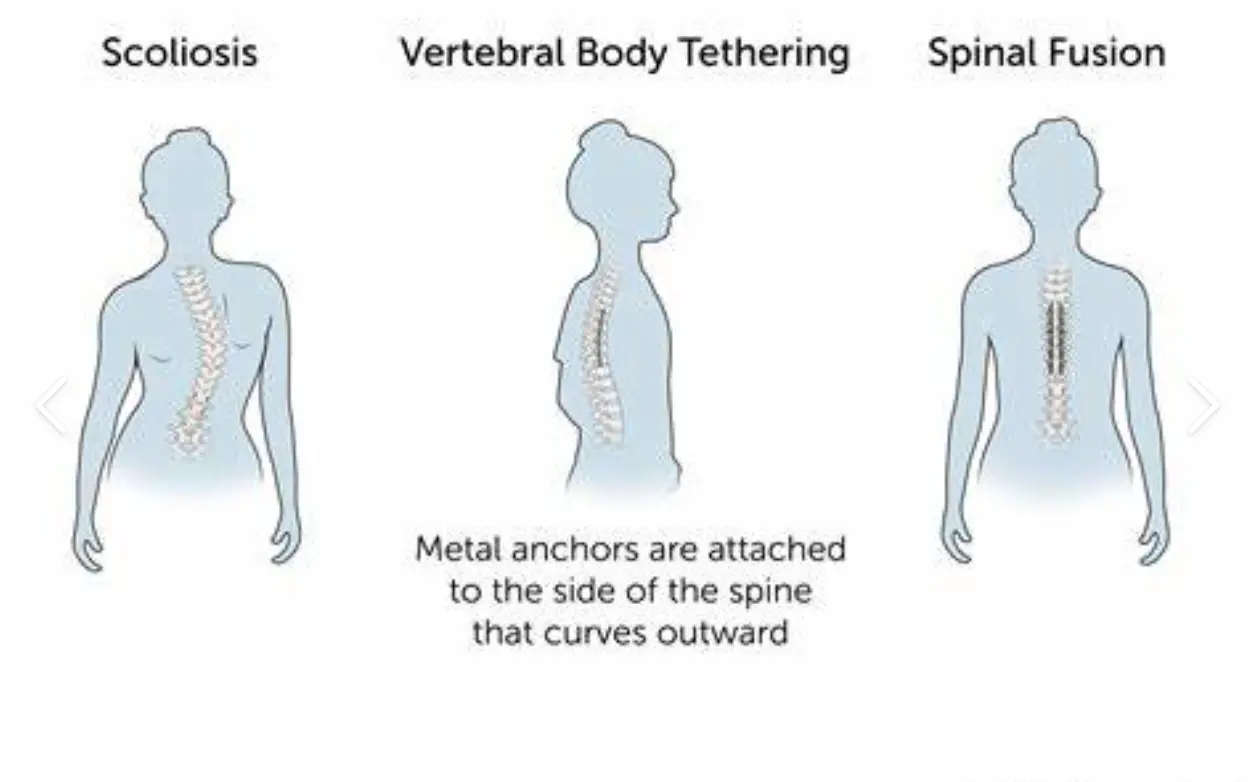
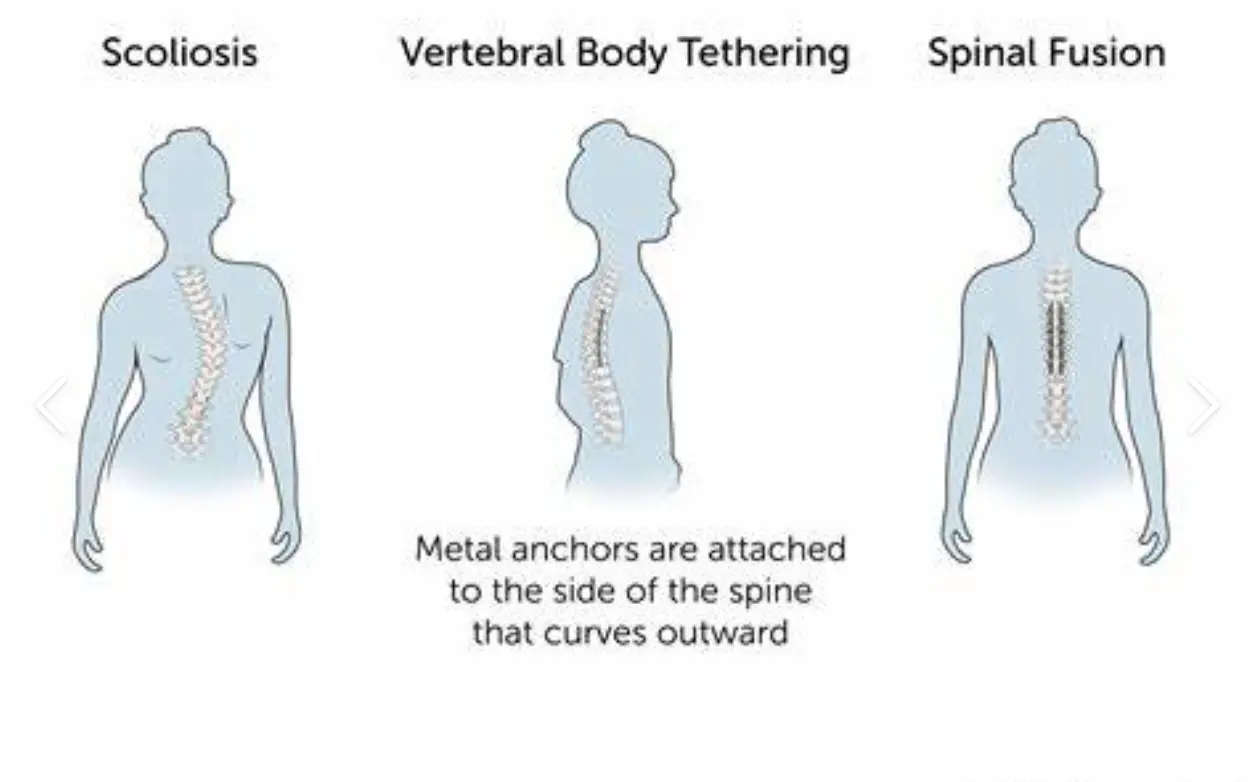
En los casos en que la curvatura es grave o sigue progresando a pesar del corsé, puede recomendarse la cirugía de fusión vertebral. Este procedimiento consiste en fusionar las vértebras mediante varillas metálicas y tornillos para enderezar la columna. Aunque la fusión vertebral puede proporcionar una corrección significativa, también limita la flexibilidad de la columna y puede dar lugar a complicaciones a largo plazo.

¿Qué es el anclaje para escoliosis?
El anclaje de la escoliosis, también conocido como anclaje del cuerpo vertebral o corrección anterior de la escoliosis, es un procedimiento quirúrgico mínimamente invasivo cuyo objetivo es corregir la curvatura de la columna conservando la flexibilidad de la misma. A diferencia de la fusión espinal, que fusiona las vértebras, el anclaje de la escoliosis utiliza una cuerda flexible para guiar el crecimiento de la columna y corregir gradualmente la curvatura.
Durante la intervención, se realizan pequeñas incisiones en el pecho o el abdomen y se fija el anclaje a las vértebras mediante tornillos o ganchos. A continuación, se aprieta el anclaje, tirando de la columna hacia una posición más alineada. Con el tiempo, a medida que el paciente crece, el anclaje permite el crecimiento controlado de un lado de la columna, corrigiendo la curvatura.
El procedimiento: Cómo funciona el anclaje para la escoliosis
La fijación de la escoliosis suele realizarse bajo anestesia general y requiere un equipo de cirujanos y profesionales médicos cualificados. El procedimiento comienza con la colocación del paciente en la mesa de operaciones y la preparación y esterilización de la zona quirúrgica.
Se realizan pequeñas incisiones en el tórax o el abdomen, dependiendo de la localización de la curvatura. A continuación, el cirujano introduce un toracoscopio o un laparoscopio, que permite visualizar la columna vertebral y las estructuras circundantes. A través de estas pequeñas incisiones, el cirujano coloca tornillos o ganchos en las vértebras y fija el anclaje.
Una vez colocado el anclaje, el cirujano lo tensa con cuidado, enderezando gradualmente la columna vertebral. Este paso requiere precisión y un control cuidadoso para garantizar que se aplica la tensión correcta. Una vez conseguida la corrección deseada, se cierran las incisiones y se traslada al paciente a la zona de recuperación.
Ventajas del anclaje para escoliosis
El anclaje para escoliosis ofrece varias ventajas sobre los tratamientos tradicionales. Una de las principales es la conservación de la flexibilidad de la columna vertebral. A diferencia de la fusión espinal, que limita la amplitud de movimiento de la columna vertebral, la fijación de la escoliosis permite un crecimiento y movimiento continuos.
Además, la fijación de la escoliosis es un procedimiento mínimamente invasivo, que permite realizar incisiones más pequeñas, reducir la pérdida de sangre y acortar la estancia hospitalaria en comparación con la cirugía de fusión espinal. Las incisiones más pequeñas también producen menos cicatrices y un tiempo de recuperación más rápido.
Además, el anclaje para escoliosis ha mostrado resultados prometedores en la corrección de la curvatura de la columna vertebral. Los estudios han demostrado mejoras significativas en la alineación de la columna y el aspecto estético, y algunos pacientes han conseguido una curvatura de la columna casi normal.
Riesgos y complicaciones de la fijación de la escoliosis
Como cualquier intervención quirúrgica, la fijación de la escoliosis conlleva ciertos riesgos y posibles complicaciones. Entre ellas, infección, hemorragia, lesiones nerviosas o daños en las estructuras circundantes durante la intervención. Además, existe el riesgo de que el anclaje se rompa o se afloje con el tiempo, lo que puede requerir una cirugía de revisión.
Es fundamental que los pacientes que estén pensando en someterse a un anclaje para escoliosis hablen de estos riesgos con su cirujano y los comparen con los posibles beneficios. Cada caso es único, y la decisión de someterse a un anclaje para escoliosis debe tomarse tras una cuidadosa reflexión y consulta con un profesional médico.
Criterios de elegibilidad para el anclaje de escoliosis
No todos los pacientes con escoliosis pueden someterse a un anclaje para escoliosis. La intervención suele recomendarse a pacientes con escoliosis idiopática de moderada a grave que no han respondido a los corsés o cuya curvatura sigue progresando a pesar del tratamiento conservador.
Además, los pacientes deben cumplir ciertos criterios, como tener suficiente crecimiento restante, una columna vertebral flexible y una curvatura susceptible de corrección mediante el anclaje. Es necesario que un especialista en escoliosis realice una evaluación exhaustiva para determinar si un paciente es un candidato adecuado para el anclaje de escoliosis.
Recuperación y rehabilitación tras el anclaje por escoliosis
Tras una intervención de fijación de la escoliosis, los pacientes suelen pasar unos días en el hospital para control y tratamiento del dolor. Pueden recetarse analgésicos para controlar las molestias durante el periodo de recuperación inicial.
Una vez dados de alta, los pacientes deberán seguir un programa de rehabilitación adaptado a sus necesidades específicas. Puede incluir ejercicios de fisioterapia para fortalecer los músculos de la espalda y mejorar la postura. Serán necesarias citas periódicas de seguimiento con el cirujano para supervisar los progresos y realizar los ajustes necesarios en el anclaje.
Es importante que los pacientes comprendan que el proceso de recuperación puede variar según la persona y el alcance de la intervención. Algunos pacientes pueden reanudar sus actividades normales en pocas semanas, mientras que otros pueden necesitar varios meses para recuperarse por completo.
Resultados a largo plazo y eficacia del anclaje para escoliosis
Todavía se están realizando estudios a largo plazo sobre la eficacia del anclaje de la escoliosis, pero los primeros resultados son prometedores. Varios estudios han informado de mejoras significativas en la alineación de la columna vertebral y el aspecto estético tras la cirugía de anclaje de la escoliosis.
Un estudio publicado en el Journal of Bone and Joint Surgery reveló que 90% de los pacientes que se sometieron a un anclaje de escoliosis consiguieron corregir su curvatura vertebral en al menos 50%. Otro estudio publicado en Spine Deformity informó de que los pacientes que se sometieron a una fijación de la escoliosis experimentaron una reducción significativa del ángulo de Cobb, que mide la gravedad de la curvatura de la columna vertebral.
Comparación de la fijación de la escoliosis con otras opciones quirúrgicas
Al considerar las opciones de tratamiento de la escoliosis, es esencial comparar el anclaje con otras opciones quirúrgicas, como la fusión espinal. La fusión espinal ha sido el tratamiento de referencia para los casos graves de escoliosis durante muchos años y tiene un historial demostrado de corrección de la curvatura de la columna vertebral.
Sin embargo, la fusión espinal conlleva limitaciones, como una menor flexibilidad de la columna y la posibilidad de complicaciones a largo plazo. La fijación de la escoliosis ofrece una alternativa más flexible, que permite seguir creciendo y moviéndose al tiempo que se consigue una corrección significativa de la curvatura.
La decisión entre la fijación de la escoliosis y la fusión espinal debe tomarse de forma individual, teniendo en cuenta las necesidades específicas del paciente, la gravedad de la curvatura y los posibles riesgos y beneficios de cada procedimiento.
Conclusiones: El futuro del tratamiento de la escoliosis
El anclaje para escoliosis representa un avance significativo en el tratamiento de la escoliosis, ya que ofrece una alternativa más flexible y menos invasiva a las opciones quirúrgicas tradicionales. Gracias a su capacidad para corregir la curvatura de la columna vertebral conservando su flexibilidad, el anclaje para la escoliosis puede revolucionar el tratamiento de la escoliosis.
Aunque todavía se están realizando estudios a largo plazo, los primeros resultados han sido prometedores en cuanto a la alineación de la columna vertebral y el aspecto estético. A medida que la tecnología siga avanzando, es probable que el anclaje para la escoliosis se convierta en una opción de tratamiento cada vez más popular y eficaz para los pacientes con escoliosis.
Sin embargo, es importante tener en cuenta que el anclaje para escoliosis no es adecuado para todos los pacientes, y cada caso debe ser evaluado individualmente por un especialista en escoliosis. La decisión de someterse a un anclaje para escoliosis debe tomarse tras considerar detenidamente los posibles riesgos y beneficios, en consulta con un profesional médico.
En conclusión, el anclaje para escoliosis ofrece una solución de vanguardia para el tratamiento de la escoliosis, proporcionando a los pacientes una opción más flexible y menos invasiva. Con la investigación en curso y los avances tecnológicos, el futuro del tratamiento de la escoliosis parece prometedor y ofrece esperanzas de mejorar los resultados y la calidad de vida de las personas con escoliosis.
Referencias
- Weinstein, S. L., Dolan, L. A., Cheng, J. C., Danielsson, A., & Morcuende, J. A. "Escoliosis idiopática del adolescente". The Lancet. 2008;371(9623):1527-1537. doi: 10.1016/S0140-6736(08)60658-3
- Negrini, S., Aulisa, A. G., Aulisa, L., et al. "Directrices SOSORT 2011: Tratamiento ortopédico y rehabilitador de la escoliosis idiopática durante el crecimiento". Escoliosis. 2012;7(1):3. doi: 10.1186/1748-7161-7-3
- Kotwicki, T., Negrini, S., Grivas, T. B., et al. "Methodology of evaluation of morphology of the spine and the trunk in idiopathic scoliosis and other spinal deformities: 6th SOSORT consensus paper". Escoliosis. 2009;4:26. doi: 10.1186/1748-7161-4-26
- Kaspiris, A., Grivas, T. B., Weiss, H. R., & Turnbull, D. "Health-related quality of life in patients with adolescent idiopathic scoliosis treated with bracing: A review". Revista de Rehabilitación Musculoesquelética y de la Espalda. 2012;25(4):219-226. doi: 10.3233/BMR-2012-0324
- Wajchenberg, M., Santos, F. P., & Puertas, E. B. "Biomecánica de la escoliosis: ¿Qué sabemos realmente?" Revista Mundial de Ortopedia. 2015;6(5):435-444. doi: 10.5312/wjo.v6.i5.435
- Ogon, M., Giesinger, J. M., Behensky, H., et al. "Health-related quality of life in idiopathic scoliosis after treatment: A comparison between brace and surgical management". Revista Bone & Joint. 2011;93-B(8):975-980. doi: 10.1302/0301-620X.93B8.26095
- Carreón, L. Y., Sanders, J. O., Diab, M., et al. "Satisfacción del paciente tras la corrección quirúrgica de la escoliosis idiopática del adolescente". Columna vertebral. 2011;36(12):965-968. doi: 10.1097/BRS.0b013e3181ef13f1
- Lonstein, J. E. "Escoliosis idiopática". Pediatría. 1994;94(5):700-703. PMID: 7936850
- Daniels, A. H., Bess, S., Line, B., et al. "Coronal plane spinal alignment: Clasificación, indicaciones y resultados". Deformidad de la columna vertebral. 2014;2(4):300-309. doi: 10.1016/j.jspd.2014.04.007
- Green, B. N., Johnson, C., & Moreau, W. J. "¿Existe una relación entre la escoliosis idiopática y la práctica de la quiropráctica? A discussion on theoretical insights and hypotheses". Quiropráctica y osteopatía. 2006;14:15. doi: 10.1186/1746-1340-14-15