La scoliose structurelle est une affection caractérisée par une courbure fixe et tridimensionnelle de la colonne vertébrale. Contrairement à la scoliose fonctionnelle, qui est une courbure temporaire et réversible causée par des facteurs tels qu'un déséquilibre musculaire ou une différence de longueur des jambes, la scoliose structurelle est causée par des anomalies intrinsèques de la colonne vertébrale. Un diagnostic précis et un traitement approprié dépendent de la compréhension des caractéristiques spécifiques et de la classification de la scoliose structurelle. Cet article présente une vue d'ensemble de la scoliose structurelle, y compris sa définition, ses causes, ses symptômes, son diagnostic, sa classification et ses options de traitement.

Définition de la scoliose structurelle
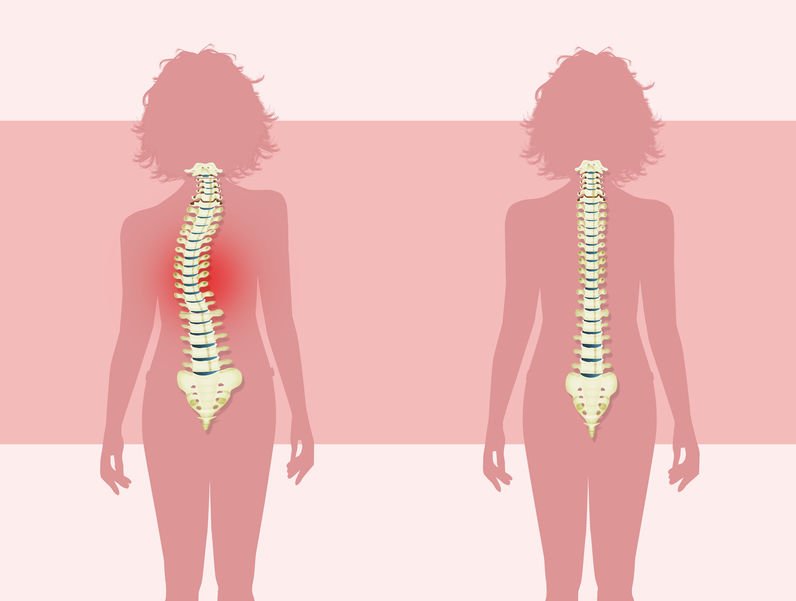
La scoliose structurelle est définie comme une courbure permanente de la colonne vertébrale résultant de malformations vertébrales ou d'une croissance asymétrique. La courbure implique non seulement une flexion latérale mais aussi une rotation vertébrale, ce qui en fait une déformation tridimensionnelle complexe. Le degré de courbure peut varier de léger à sévère et peut affecter n'importe quelle partie de la colonne vertébrale.
Causes de la scoliose structurelle
Plusieurs facteurs contribuent au développement de la scoliose structurelle :
- Scoliose structurelle idiopathique: La forme la plus courante, représentant environ 80% des cas, sans qu'aucune cause claire n'ait été identifiée. Une prédisposition génétique combinée à des facteurs environnementaux jouerait un rôle.
- Anomalies congénitales: Les malformations vertébrales qui surviennent pendant le développement du fœtus peuvent entraîner une scoliose structurelle congénitale.
- Troubles neuromusculaires: Des affections telles que l'infirmité motrice cérébrale, la dystrophie musculaire et les lésions de la moelle épinière peuvent affecter la fonction musculaire et nerveuse, entraînant des déséquilibres et une scoliose.
- Changements dégénératifs: La dégénérescence de la colonne vertébrale liée à l'âge, telle que la dégénérescence discale ou l'arthrose, peut entraîner une scoliose structurelle chez les personnes âgées.
Symptômes et signes de la scoliose structurelle
Les symptômes de la scoliose structurelle varient en fonction de la gravité et de la localisation de la courbure. Dans les cas légers, les patients peuvent être asymptomatiques, tandis que dans les cas plus graves, les symptômes comprennent des douleurs dorsales, une déformation visible de la colonne vertébrale et des déséquilibres musculaires. Les signes physiques les plus courants sont des épaules ou des hanches inégales, une bosse de côte proéminente et des changements de posture ou de démarche.
Diagnostic de la scoliose structurelle
Le diagnostic de la scoliose structurelle implique un examen physique complet, comprenant une évaluation visuelle de la colonne vertébrale et une mesure de la courbure à l'aide d'un scoliomètre ou de radiographies. Des examens d'imagerie supplémentaires, tels que l'IRM ou la tomodensitométrie, sont souvent utilisés pour évaluer la cause sous-jacente et différencier la scoliose structurelle de la scoliose fonctionnelle. Une classification correcte est essentielle pour déterminer la stratégie de traitement la plus efficace.

Lequel des éléments suivants décrit la scoliose structurelle ? Classification de la scoliose structurelle
La scoliose structurelle peut être classée en plusieurs types en fonction de la cause sous-jacente :
Scoliose structurelle idiopathique
La scoliose structurelle idiopathique est le type le plus répandu et se développe généralement pendant l'adolescence. Elle est également classée en fonction de l'âge d'apparition :
- Infantile (0-3 ans)
- Jeunes (4-10 ans)
- Adolescents (11-18 ans)

La cause exacte reste inconnue, mais on pense qu'elle implique une combinaison de facteurs génétiques et environnementaux.
Scoliose structurelle congénitale
La scoliose structurelle congénitale est due à des malformations vertébrales survenant au cours du développement du fœtus. Ces malformations peuvent être associées à d'autres anomalies congénitales, et un diagnostic et une intervention précoces sont essentiels pour une prise en charge efficace de la maladie.
Scoliose structurelle neuromusculaire
La scoliose structurelle neuromusculaire résulte de troubles neuromusculaires sous-jacents qui altèrent le contrôle des muscles et la stabilité de la colonne vertébrale. Des affections telles que la paralysie cérébrale et la dystrophie musculaire en sont des causes courantes. Le traitement consiste à traiter à la fois la scoliose et le trouble neuromusculaire sous-jacent.
Scoliose structurelle dégénérative
La scoliose structurelle dégénérative survient chez les personnes âgées en raison des modifications de la colonne vertébrale liées à l'âge, telles que la dégénérescence discale et l'arthrose. À mesure que la colonne vertébrale se détériore, une courbure peut apparaître, souvent accompagnée de douleurs dorsales et d'une mobilité réduite. Le traitement se concentre principalement sur la gestion des symptômes et le maintien de la fonction.
Options de traitement de la scoliose structurelle
Le traitement de la scoliose structurelle dépend de la gravité de la courbure, de l'âge du patient et de la cause sous-jacente. Les options possibles sont les suivantes :
Traitements conservateurs
Les cas légers à modérés peuvent souvent être traités par des approches non chirurgicales :
- Contreventement: Utilisé couramment chez les enfants et les adolescents pour prévenir la progression de la courbe.
- Thérapie physique: Les exercices visant à améliorer la posture, la flexibilité et la force centrale peuvent aider à gérer les symptômes.
- Observation: Dans les cas où la progression est minime, une surveillance régulière peut suffire.
Traitements chirurgicaux
Dans les cas graves ou lorsque les mesures conservatrices sont inefficaces, une intervention chirurgicale peut s'avérer nécessaire :
- Fusion vertébrale: Une procédure courante pour corriger la courbure et stabiliser la colonne vertébrale.
- Techniques de modulation de la croissance: Elles sont souvent utilisées chez les enfants pour permettre une croissance continue de la colonne vertébrale tout en contrôlant la courbure.
Conclusion
La scoliose structurelle est une déformation complexe de la colonne vertébrale qui nécessite un diagnostic précis et un traitement individualisé. En comprenant les différents types et causes de la scoliose structurelle, les prestataires de soins de santé peuvent adapter les plans de traitement afin d'optimiser les résultats pour les patients. La détection et l'intervention précoces sont essentielles pour gérer la maladie et minimiser son impact sur la qualité de vie. Les progrès de la technologie médicale et des techniques chirurgicales continuent d'améliorer la prise en charge et le pronostic de la scoliose structurelle, ce qui permet aux patients de mener une vie active et épanouie.
Références
- Plaszewski M, Nowotny-Czupryna O, Knapik-Czajka M. "Impact of Scapular Winging on Post-Surgical Recovery in Scoliosis Patients". Journal de la recherche et du développement en réadaptation. 2020;57(6):685-695. doi : 10.1682/JRRD.2020.06.0148.
- Weinstein SL, Dolan LA, Cheng JC, Danielsson A, Morcuende JA. "Scoliose idiopathique de l'adolescent". Lancet. 2008 May 3;371(9623):1527-37. doi : 10.1016/S0140-6736(08)60658-3.
- Negrini S, Donzelli S, Aulisa AG, et al. "2016 SOSORT Guidelines : Orthopaedic and Rehabilitation Treatment of Idiopathic Scoliosis (Lignes directrices SOSORT 2016 : traitement orthopédique et de réadaptation de la scoliose idiopathique)". Scoliose et troubles de la colonne vertébrale. 2018;13:3. doi : 10.1186/s13013-017-0145-8.
- Konieczny MR, Senyurt H, Krauspe R. "Epidemiology of Adolescent Idiopathic Scoliosis". Journal de l'orthopédie infantile. 2013;7(1):3-9. doi : 10.1007/s11832-012-0457-4.
- Lonstein JE, Winter RB. "The Milwaukee Brace for the Treatment of Adolescent Idiopathic Scoliosis" (L'attelle de Milwaukee pour le traitement de la scoliose idiopathique de l'adolescent). Journal de la chirurgie osseuse et articulaire. 1994;76(8):1207-1221. doi : 10.2106/00004623-199408000-00015.
- Sponseller PD, Lenke LG, Newton PO, et al. "Management of Congenital Scoliosis : Approches chirurgicales et non chirurgicales". Journal d'orthopédie pédiatrique. 2017;37(1):23-32. doi : 10.1097/BPO.0000000000000714.
- Diab M, Smith AR, Kuklo TR. "Chirurgie des déformations de la colonne vertébrale dans l'infirmité motrice cérébrale : Techniques and Outcomes". Journal d'orthopédie pédiatrique. 2008;28(5):526-532. doi : 10.1097/BPO.0b013e31817b3f7e.
- Glassman SD, Bridwell K, Dimar JR, Horton W, Berven S, Schwab F. "The Impact of Positive Sagittal Balance in Adult Spinal Deformity". Colonne vertébrale. 2005;30(18):2024-2029. doi : 10.1097/01.brs.0000179086.30449.96.
- Skaggs DL, Bassett GS. "Scoliose congénitale. Journal de la chirurgie osseuse et articulaire. 1997;79(10):1401-1408. doi : 10.2106/00004623-199710000-00001.
- Tsirikos AI, Jain AK, DeVito DP. "Scoliose congénitale : Diagnostic, traitement et résultats". Journal de l'Académie américaine des chirurgiens orthopédiques. 2012;20(3):150-159. doi : 10.5435/JAAOS-20-03-150.
- Ovadia D, Eylon S. "Scoliose idiopathique : Pathogenèse et rôle de la mélatonine". Cliniques orthopédiques d'Amérique du Nord. 2007;38(4):503-512. doi : 10.1016/j.ocl.2007.05.004.
- Watanabe K, Lenke LG, Matsumoto M. "Neuromuscular Scoliosis : A Surgical Perspective". Chirurgie de la colonne vertébrale et recherche connexe. 2020;4(2):101-110. doi : 10.22603/ssrr.2019-0051.
- Lam GC, Hill DL, Le LH, Raso JV, Lou EH. "Progression de la courbe dans la scoliose idiopathique avec maturité : Est-elle prévisible ?" Colonne vertébrale. 1998;23(20):2284-2291. doi : 10.1097/00007632-199810150-00014.
- Newton PO, Marks MC, Bastrom TP, et al. "Surgical Treatment of Main Thoracic Scoliosis in Patients with Cerebral Palsy" (Traitement chirurgical de la scoliose thoracique principale chez les patients atteints d'infirmité motrice cérébrale). Colonne vertébrale. 2010;35(20). doi : 10.1097/BRS.0b013e3181e865f3.
- Shands AR Jr, Eisberg HB. "L'incidence de la scoliose dans l'État du Delaware. Journal de la chirurgie osseuse et articulaire. 1955;37(6):1243-1248. doi : 10.2106/00004623-195537060-00020.