Neuromuscular scoliosis is a complex spinal deformity that occurs as a result of underlying neuromuscular conditions such as cerebral palsy, muscular dystrophy, or spinal cord injury. It is characterized by an abnormal curvature of the spine, which can lead to significant functional limitations and health complications. Accurate coding of neuromuscular scoliosis is crucial for proper documentation, billing, and reimbursement in healthcare settings. In this article, we will explore the key guidelines and examples for accurately coding neuromuscular scoliosis using the International Classification of Diseases, Tenth Revision (ICD-10).

Understanding ICD-10 Coding for Neuromuscular Scoliosis
ICD-10 is a standardized system used worldwide for classifying diseases, injuries, and other health conditions. It provides a comprehensive set of codes that allow healthcare providers to accurately document and communicate diagnoses. When it comes to coding neuromuscular scoliosis, it is essential to understand the specific guidelines and codes associated with this condition.
Key Guidelines for Accurate Coding of Neuromuscular Scoliosis
To accurately code neuromuscular scoliosis, it is important to follow certain guidelines. Firstly, it is crucial to identify the underlying neuromuscular condition causing the scoliosis. This information helps in selecting the appropriate ICD-10 code. Secondly, it is important to document the severity of the scoliosis, as this can impact the choice of code. Lastly, it is essential to document any associated symptoms or complications that may be present, as these can also affect the coding process.
Differentiating Neuromuscular Scoliosis from Other Types
Neuromuscular scoliosis must be differentiated from other types of scoliosis, such as idiopathic or congenital scoliosis. Idiopathic scoliosis occurs without an identifiable cause, while congenital scoliosis is present at birth due to abnormal spinal development. Differentiating between these types is crucial for accurate coding and appropriate treatment planning.
Coding Neuromuscular Scoliosis Based on Underlying Conditions
Neuromuscular scoliosis can be caused by various underlying conditions, each requiring a specific ICD-10 code. For example, if the scoliosis is due to cerebral palsy, the appropriate code would be G80.8 (Other cerebral palsy). Similarly, if the scoliosis is associated with muscular dystrophy, the code would be G71.0 (Muscular dystrophy). It is important to review the ICD-10 coding manual for the complete list of codes associated with different neuromuscular conditions.
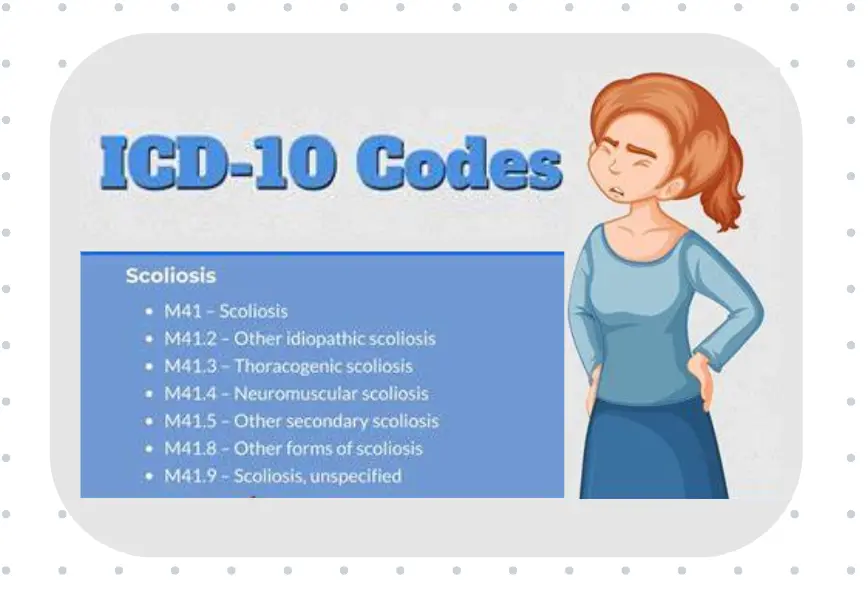
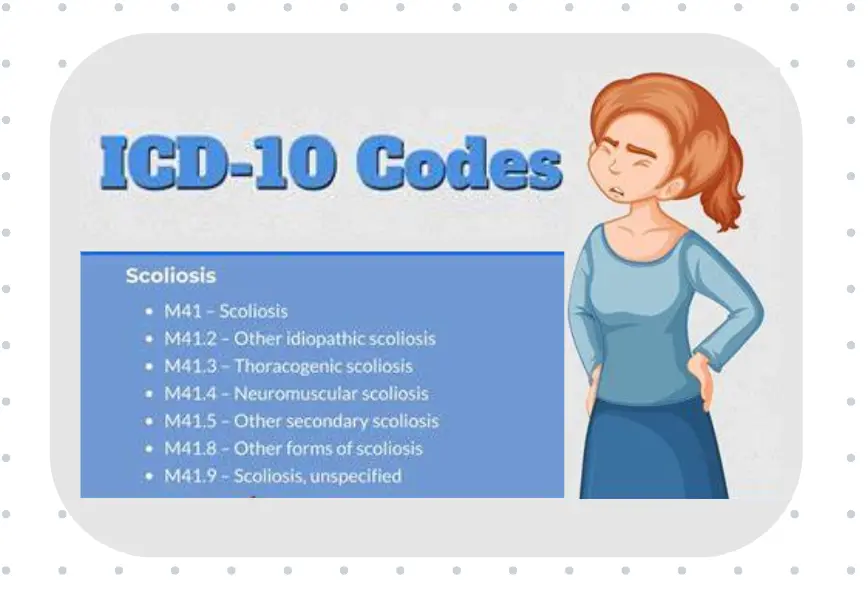
Specific ICD-10 Codes for Neuromuscular Scoliosis
ICD-10 provides specific codes for different types and severities of scoliosis. For neuromuscular scoliosis, the codes fall under the M41 category (Scoliosis). The specific code to be used depends on factors such as the location of the scoliosis, the severity of the curvature, and any associated complications. For example, M41.5 (Other idiopathic scoliosis) is used for scoliosis of the thoracolumbar region, while M41.8 (Other forms of scoliosis) is used for scoliosis of other specified sites.
Coding Neuromuscular Scoliosis in Pediatric Patients
Neuromuscular scoliosis is commonly seen in pediatric patients with underlying neuromuscular conditions. Accurate coding in this population is crucial for appropriate treatment planning and monitoring. When coding neuromuscular scoliosis in pediatric patients, it is important to consider the age of onset, the severity of the scoliosis, and any associated complications. Additionally, it is important to document any growth-related changes in the curvature, as this can impact the choice of code.
Coding Neuromuscular Scoliosis in Adult Patients
While neuromuscular scoliosis is more commonly seen in pediatric patients, it can also occur in adults with underlying neuromuscular conditions. Accurate coding in adult patients requires consideration of factors such as the duration of the scoliosis, the impact on daily functioning, and any associated degenerative changes in the spine. It is important to document any changes in the curvature over time and any worsening of symptoms to ensure accurate coding.
Common Challenges in Coding Neuromuscular Scoliosis
Coding neuromuscular scoliosis can present certain challenges. One common challenge is the lack of specificity in the documentation. Healthcare providers must ensure that the documentation clearly identifies the underlying neuromuscular condition causing the scoliosis. Another challenge is the complexity of the coding system itself. It is important for coders to stay updated with the latest ICD-10 guidelines and codes to accurately assign the appropriate codes.
Documentation Requirements for Accurate Coding
Accurate coding of neuromuscular scoliosis relies heavily on comprehensive and detailed documentation. Healthcare providers must document the underlying neuromuscular condition, the severity of the scoliosis, any associated symptoms or complications, and any changes in the curvature over time. Additionally, it is important to document any diagnostic tests or imaging studies performed to support the diagnosis.
Examples of Accurate ICD-10 Coding for Neuromuscular Scoliosis
To illustrate accurate coding for neuromuscular scoliosis, let’s consider an example. A pediatric patient with cerebral palsy presents with severe scoliosis of the thoracic spine. The appropriate ICD-10 code for this case would be G80.8 (Other cerebral palsy) and M41.5 (Other idiopathic scoliosis). This coding accurately reflects the underlying neuromuscular condition and the specific type and location of the scoliosis.
Conclusion and Importance of Accurate Coding in Neuromuscular Scoliosis
Accurate coding of neuromuscular scoliosis is essential for proper documentation, billing, and reimbursement in healthcare settings. It allows for appropriate treatment planning, monitoring, and research. By following the key guidelines and using the specific ICD-10 codes associated with neuromuscular scoliosis, healthcare providers can ensure accurate coding and improve the overall quality of care for patients with this complex condition.
Références
- King HA, Johnston CE, Drennan JC. “Scoliosis in cerebral palsy.” J Pediatr Orthop. 1983;3(3):244-247. doi: 10.1097/01241398-198305000-00006
- Janicki JA, Narayanan UG, Cahill PJ, Saldanha KA, Miyanji F. “Management of neuromuscular scoliosis with growth-friendly implants: indications and outcomes.” J Am Acad Orthop Surg. 2021;29(18):790-798. doi: 10.5435/JAAOS-D-20-00971
- Vitale MG, Levy DE, Johnson MG, Matsumoto H, Choe JC, Hyman JE. “Assessment of health status in children with cerebral palsy after treatment for scoliosis with posterior spinal fusion.” J Bone Joint Surg Am. 2006;88(6):1212-1219. doi: 10.2106/JBJS.E.00169
- Sponseller PD, Jain A, Yaszay B, et al. “Posterior spinal fusion for neuromuscular scoliosis: outcomes and complications in 201 patients.” J Bone Joint Surg Am. 2013;95(10):932-938. doi: 10.2106/JBJS.L.01129
- McCarthy RE, Luhmann S. “Neuromuscular scoliosis.” Orthop Clin North Am. 1999;30(3):435-449. doi: 10.1016/S0030-5898(05)70028-4
- Bowen RE, Scaduto AA. “The role of bracing in neuromuscular scoliosis.” J Am Acad Orthop Surg. 2012;20(4):242-249. doi: 10.5435/JAAOS-20-04-242
- Vitale MG, Roye DP Jr. “Scoliosis in cerebral palsy: the role of spinal surgery.” J Am Acad Orthop Surg. 2006;14(6):367-375. doi: 10.5435/00124635-200606000-00007
- Tsirikos AI, Mains E, Dunsmuir RA, Banaszkiewicz PA, Turnbull JE. “Surgical correction of scoliosis in Duchenne muscular dystrophy using pedicle screw instrumentation.” Spine (Phila Pa 1976). 2012;37(7). doi: 10.1097/BRS.0b013e318240e1c2
- van Bosse HJP, Thompson GH. “Severe scoliosis in patients with cerebral palsy: tips and tricks in surgical management.” J Child Orthop. 2013;7(5):425-433. doi: 10.1007/s11832-013-0516-4
- Sussman MD. “Scoliosis in the child with a motor disability.” Orthop Clin North Am. 1999;30(3):445-465. doi: 10.1016/S0030-5898(05)70029-6
- Persson-Bunke M, Hägglund G, Lauge-Pedersen H, Czuba T, Nordmark E. “Scoliosis in a total population of children with cerebral palsy.” Spine (Phila Pa 1976). 2012;37(12). doi: 10.1097/BRS.0b013e31824c02a2
- Tsirikos AI, Lipton G, Chang WN, Dabney KW, Miller F. “Surgical correction of spinal deformity in patients with cerebral palsy using the unit rod instrumentation.” Spine (Phila Pa 1976). 2008;33(10):1133-1140. doi: 10.1097/BRS.0b013e31816a8dd4
- Oda JE, Samdani AF, Hwang SW, et al. “Risk factors for complications in spinal deformity surgery in children with cerebral palsy: a retrospective study of 352 cases.” Déformation de la colonne vertébrale. 2017;5(4):288-295. doi: 10.1016/j.jspd.2017.02.006
- Berven SH, Lowe TG. “Neuromuscular scoliosis: causes of deformity and principles for evaluation and management.” Semin Spine Surg. 2001;13(2):85-95. doi: 10.1053/j.semss.2000.00016
- Sanders JO, Baumann R, Brown D, et al. “Spinal deformity in Duchenne muscular dystrophy: an overview of management.” J Pediatr Orthop. 2002;22(5):735-739. doi: 10.1097/01241398-200209000-00035