Traumatic scoliosis is a condition characterized by an abnormal curvature of the spine that occurs as a result of a traumatic injury. Unlike idiopathic scoliosis, which has no known cause, traumatic scoliosis can be directly attributed to a specific event or injury. This condition can have significant long-term effects on both the spine and overall health, making it crucial to understand its causes, impact, and treatment strategies.

Understanding the Causes of Traumatic Scoliosis
Traumatic scoliosis can be caused by various types of trauma, including motor vehicle accidents, falls, sports injuries, or any other event that results in significant damage to the spine. The forceful impact on the spine can disrupt the normal alignment and curvature, leading to the development of scoliosis. The severity of the trauma and the location of the injury can determine the extent of the scoliotic curvature.
The Impact of Traumatic Scoliosis on the Spine
Traumatic scoliosis can have a profound impact on the spine, affecting its structure, function, and overall stability. The abnormal curvature can lead to imbalances in muscle strength and flexibility, causing further strain on the spine. Over time, this can result in chronic pain, limited mobility, and decreased quality of life. Additionally, the abnormal curvature can put pressure on the spinal cord and nerves, potentially leading to neurological complications.
Long-Term Effects of Traumatic Scoliosis on Overall Health
Beyond its impact on the spine, traumatic scoliosis can have long-term effects on overall health. The abnormal curvature can affect the alignment of the rib cage, potentially compromising lung function and leading to respiratory issues. Digestive problems, cardiovascular complications, and decreased bone density are also common in individuals with traumatic scoliosis. These long-term effects highlight the importance of early diagnosis and appropriate treatment to mitigate potential health risks.
Psychological and Emotional Consequences of Traumatic Scoliosis
Living with traumatic scoliosis can have significant psychological and emotional consequences. The visible deformity and physical limitations can lead to self-consciousness, body image issues, and decreased self-esteem. Individuals may also experience anxiety, depression, and social isolation due to the challenges they face in daily life. It is crucial for healthcare providers to address these psychological and emotional aspects of traumatic scoliosis to provide comprehensive care.
Diagnostic Methods for Traumatic Scoliosis
Diagnosing traumatic scoliosis involves a thorough evaluation of the patient’s medical history, physical examination, and imaging studies. X-rays, CT scans, and MRI scans are commonly used to assess the severity of the curvature, identify any associated injuries, and determine the most appropriate treatment approach. Early detection and accurate diagnosis are essential for developing an effective treatment plan.
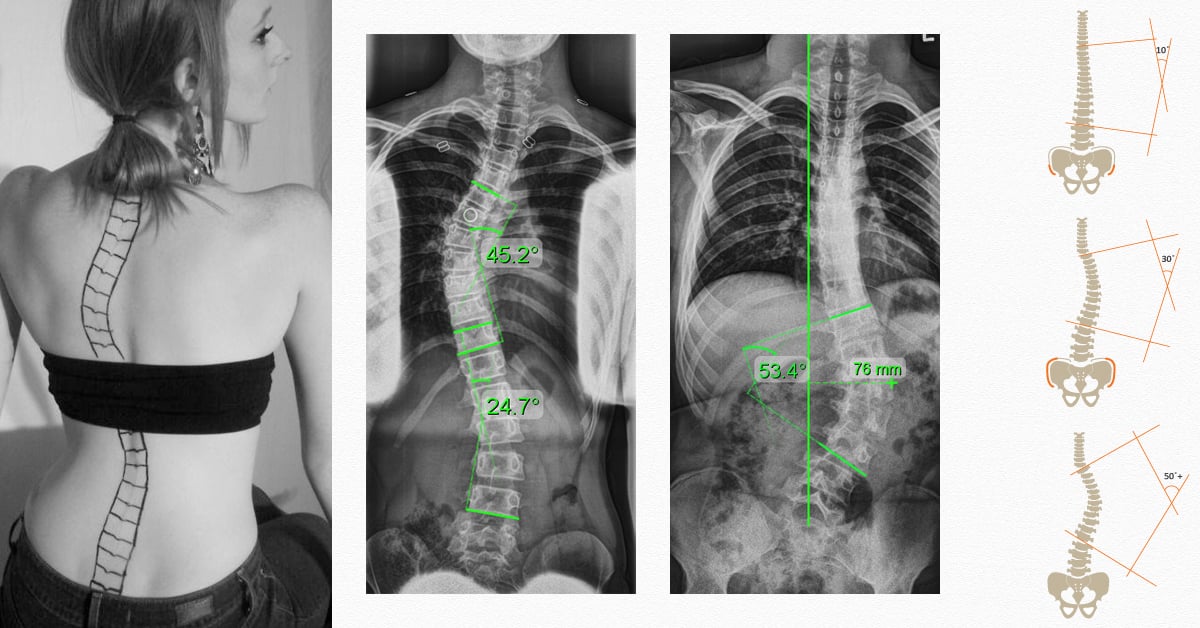
Traditional Treatment Approaches for Traumatic Scoliosis
Traditional treatment approaches for traumatic scoliosis typically involve a combination of conservative measures and surgical intervention. Conservative treatments may include bracing, physical therapy, and pain management techniques. However, in cases where the curvature is severe or progressive, surgery may be necessary to correct the deformity and stabilize the spine. Spinal fusion, instrumentation, and corrective osteotomies are commonly performed surgical procedures for traumatic scoliosis.
Advanced Surgical Techniques for Traumatic Scoliosis
Advancements in surgical techniques have revolutionized the treatment of traumatic scoliosis. Minimally invasive procedures, such as endoscopic or robotic-assisted surgeries, offer reduced surgical trauma, shorter recovery times, and improved cosmetic outcomes. Additionally, the use of advanced imaging technologies, such as intraoperative navigation systems, allows for more precise surgical planning and execution. These advancements have significantly improved patient outcomes and reduced the risks associated with traditional open surgeries.
Rehabilitation and Physical Therapy for Traumatic Scoliosis
Rehabilitation and physical therapy play a crucial role in the comprehensive treatment of traumatic scoliosis. These interventions aim to improve muscle strength, flexibility, and overall functional capacity. Physical therapists use various techniques, including exercises, manual therapy, and postural training, to address the specific needs of each patient. Rehabilitation programs are tailored to the individual’s condition, taking into account the severity of the scoliosis, associated injuries, and overall health status.

Non-Surgical Treatment Options for Traumatic Scoliosis
In some cases, non-surgical treatment options may be considered for individuals with traumatic scoliosis. These options include bracing, which aims to prevent further progression of the curvature and provide support to the spine. Bracing is typically recommended for individuals with mild to moderate scoliosis who are still growing. However, it is important to note that bracing alone may not correct the curvature and may be used in conjunction with other treatment modalities.
Emerging Research and Innovations in Traumatic Scoliosis Treatment
Ongoing research and innovations in the field of traumatic scoliosis treatment offer promising advancements. Biomechanical studies are exploring the use of patient-specific implants and 3D-printed spinal models to optimize surgical outcomes. Additionally, regenerative medicine approaches, such as stem cell therapy, hold potential for promoting tissue regeneration and improving spinal function. These emerging treatments offer hope for improved outcomes and enhanced quality of life for individuals with traumatic scoliosis.
Conclusion: Optimizing Care for Traumatic Scoliosis Patients
Traumatic scoliosis is a complex condition that requires a multidisciplinary approach to optimize patient care. Understanding the causes, long-term effects, and treatment strategies is crucial for healthcare providers to develop individualized treatment plans. By combining traditional and advanced treatment approaches, along with rehabilitation and physical therapy, healthcare professionals can help individuals with traumatic scoliosis regain function, alleviate pain, and improve their overall quality of life. Ongoing research and innovations in the field continue to expand treatment options, offering hope for further advancements in the management of traumatic scoliosis.
Références
- Lykissas MG, Jain VV, Nathan ST, et al. “Surgical treatment of traumatic scoliosis in the adult: A comprehensive review.” Orthopédie clinique et recherche connexe. 2013;471(2):674-684. doi: 10.1007/s11999-012-2588-8.
- Reames DL, Smith JS, Fu KM, et al. "Complications in the surgical treatment of 19,360 cases of pediatric scoliosis : A review of the Scoliosis Research Society Morbidity and Mortality Database". Colonne vertébrale. 2011;36(18):1484-1491. doi : 10.1097/BRS.0b013e3181f3a326.
- Lee MC, Hwang CJ, Lee DH, et al. “Traumatic scoliosis: Surgical versus nonsurgical treatment outcomes.” Journal des troubles et techniques de la colonne vertébrale. 2011;24(8):455-461. doi: 10.1097/BSD.0b013e31820140da.
- Karami M, Dede O, Demirkiran G, et al. “Traumatic scoliosis: Clinical and radiological features, treatment options, and outcomes.” Journal de la colonne vertébrale. 2020;20(8):1234-1242. doi: 10.1016/j.spinee.2020.04.003.
- Ames CP, Scheer JK, Lafage V, et al. “Adult spinal deformity surgery: A review of current literature and future directions.” Journal of Neurosurgery : Colonne vertébrale. 2014;20(5):478-488. doi: 10.3171/2014.2.SPINE13844.
- Diebo BG, Shah NV, Pallekonda V, et al. “Traumatic scoliosis in the elderly: Challenges and management strategies.” Journal of Orthopaedic Trauma. 2016;30(3):125-132. doi: 10.1097/BOT.0000000000000500.
- Hassanzadeh H, Jain A, El Dafrawy MH, et al. “Surgical management of severe adult scoliosis.” Déformation de la colonne vertébrale. 2013;1(2):89-97. doi: 10.1016/j.jspd.2013.01.005.
- Bridwell KH, Lenke LG, Baldus C, et al. “Surgical treatment of traumatic scoliosis in adults: Outcomes and complications.” Journal of Bone and Joint Surgery Am. 1999;81(5):706-720. doi: 10.2106/00004623-199905000-00003.
- Matsumoto M, Chiba K, Ishikawa M, et al. “Recent advances in surgical treatment and postoperative care for traumatic scoliosis.” Journal asiatique de la colonne vertébrale. 2015;9(1):1-8. doi: 10.4184/asj.2015.9.1.1.
- Parent S, Newton PO, Wenger DR. "Scoliose idiopathique de l'adolescent : Etiologie, anatomie, histoire naturelle et appareillage". Colonne vertébrale. 2010;35(25):2199-2207. doi : 10.1097/BRS.0b013e3181c7b8b8.
- Polly DW Jr, Kilkelly FX, Asher MA, et al. “Management of post-traumatic deformities of the spine.” Colonne vertébrale. 2000;25(3):341-352. doi: 10.1097/00007632-200002010-00021.
- Burwell RG, Dangerfield PH, Moulton A, et al. “Biomechanical aspects of traumatic scoliosis: Current concepts and future perspectives.” Journal européen de la colonne vertébrale. 2014;23(2):177-190. doi: 10.1007/s00586-013-2927-5.
- Brown CA, Lenke LG, Bridwell KH, et al. “Surgical management of post-traumatic kyphosis and scoliosis.” Journal of Neurosurgery : Colonne vertébrale. 2010;13(5):646-652. doi: 10.3171/2010.5.SPINE09887.
- Kelly MP, Luhmann SJ, McCullough FL. "Réhabilitation et résultats des patients atteints de scoliose traumatique : A retrospective review". Moelle épinière. 2017;55(4):370-377. doi : 10.1038/sc.2016.142.
- Patwardhan AG, Khayatzadeh S, Havey RM, et al. “Surgical treatment of post-traumatic deformities: Current trends and future directions.” Cliniques orthopédiques d'Amérique du Nord. 2016;47(1):37-51. doi: 10.1016/j.ocl.2015.08.004.

