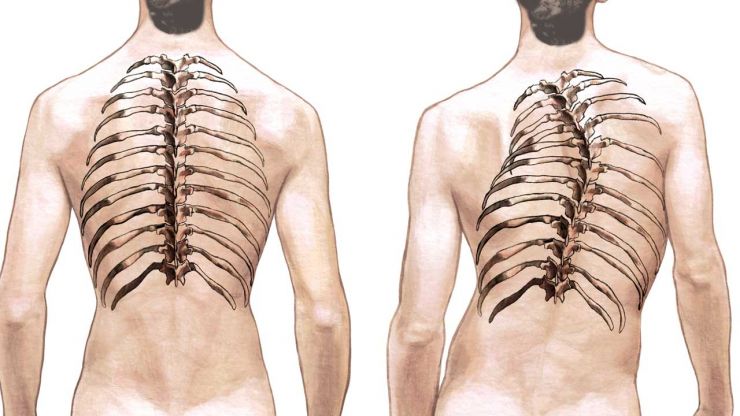
Scoliose La scoliose est une affection caractérisée par une courbure anormale de la colonne vertébrale, qui peut entraîner des complications au-delà de la colonne vertébrale elle-même. L'une des déformations notables associées à la scoliose est l'inégalité de la cage thoracique, où la courbure de la colonne vertébrale provoque une asymétrie visible de la cage thoracique. Cet article examine les causes, les symptômes et les options de traitement disponibles pour les personnes atteintes de scoliose à cage thoracique irrégulière, en soulignant l'importance d'une détection et d'une intervention précoces.

Comprendre la déformation de la cage thoracique en cas de scoliose
La scoliose à cage thoracique inégale survient lorsque la courbure de la colonne vertébrale se répercute sur les côtes, provoquant leur rotation et leur asymétrie. Cette affection est le plus souvent observée dans les cas où la scoliose affecte la région thoracique (haut du dos) de la colonne vertébrale. Lorsque la colonne vertébrale se courbe latéralement, elle fait tourner les côtes, ce qui fait qu'un côté de la cage thoracique apparaît plus proéminent que l'autre.
Causes et facteurs de risque de la scoliose irrégulière de la cage thoracique
La cause principale de la scoliose de la cage thoracique inégale est la suivante scoliose idiopathiqueLa cause exacte de cette maladie est inconnue, mais on pense qu'elle est d'origine génétique. D'autres facteurs contribuent à la maladie :
- Scoliose congénitale: Présente à la naissance en raison d'anomalies vertébrales.
- Scoliose neuromusculaire: Liées à des pathologies telles que l'infirmité motrice cérébrale ou la dystrophie musculaire .
- Scoliose dégénérative: Fréquente chez les personnes âgées en raison de l'usure de la colonne vertébrale.
Les facteurs de risque comprennent les antécédents familiaux de scoliose, le fait d'être une femme et une croissance rapide pendant l'adolescence.
Identification des symptômes et diagnostic de la scoliose à cage thoracique irrégulière
Le principal symptôme est l'asymétrie visible de la cage thoracique, un côté apparaissant généralement plus haut ou plus proéminent. D'autres symptômes peuvent apparaître :
- Mal de dos
- Difficultés respiratoires
- Réduction de la capacité pulmonaire

Le diagnostic repose sur un examen physique, des examens d'imagerie (radiographies, IRM) et la mesure de la courbure à l'aide de l'angle de Cobb pour déterminer la gravité.
Importance de la détection et de l'intervention précoces
La détection précoce est essentielle à la prise en charge de la scoliose irrégulière de la cage thoracique. L'identification précoce de la maladie permet d'intervenir à temps, ce qui peut ralentir ou arrêter la progression de la courbure de la colonne vertébrale et minimiser la déformation de la cage thoracique. Des études montrent qu'une intervention précoce peut améliorer de manière significative les résultats à long terme et la qualité de vie.
Approches non chirurgicales de la prise en charge de la scoliose irrégulière de la cage thoracique
Les traitements non chirurgicaux constituent souvent la première ligne de défense, en particulier dans les cas légers à modérés. Il s'agit notamment des traitements suivants
- Thérapie physique et exercice: Des programmes sur mesure peuvent renforcer les muscles qui soutiennent la colonne vertébrale, améliorer la posture et réduire l'inconfort.
- Contreventement: Pour les adolescents encore en phase de croissance, le port d'une attelle peut prévenir l'aggravation de la courbure et de la déformation de la cage thoracique.
Thérapie physique et exercices pour la déformation de la cage thoracique
La thérapie se concentre sur des exercices qui ciblent la stabilité du tronc, la correction de la posture et la flexibilité. Des techniques telles que la thérapie de Schroth se sont avérées efficaces pour améliorer l'alignement de la colonne vertébrale et réduire la proéminence des côtes. La thérapie manuelle et les exercices d'étirement peuvent également améliorer la mobilité et soulager la douleur.

Les techniques de haubanage et leur efficacité
Le port d'un appareil orthopédique est généralement recommandé à l'adolescence, lorsque les poussées de croissance peuvent aggraver la scoliose. Les attelles telles que l'attelle de Boston sont couramment utilisées et peuvent être efficaces pour prévenir la progression de la courbe si elles sont portées conformément à la prescription. L'observance et la bonne adaptation sont des facteurs clés pour déterminer le succès d'un appareil orthopédique.

Options chirurgicales pour corriger une scoliose irrégulière de la cage thoracique
Lorsque les interventions non chirurgicales échouent ou que la déformation est grave, une correction chirurgicale peut s'avérer nécessaire. Fusion vertébrale est l'intervention chirurgicale la plus courante. Elle consiste à fusionner des vertèbres à l'aide de tiges et de vis métalliques afin de stabiliser et de redresser la colonne vertébrale. Cette intervention peut réduire de manière significative la déformation de la cage thoracique.
Récupération et rééducation après une chirurgie de la cage thoracique
Les soins post-opératoires impliquent le port d'une attelle ou d'un plâtre pour soutenir la colonne vertébrale pendant la convalescence. La kinésithérapie est essentielle pour retrouver de la force, améliorer la souplesse et augmenter progressivement le niveau d'activité. La rééducation permet également de gérer la douleur et les problèmes psychologiques qui peuvent survenir après l'opération.
Gestion à long terme et soins de suivi
La prise en charge continue comprend des examens réguliers pour contrôler la stabilité de la colonne vertébrale, évaluer la symétrie de la cage thoracique et ajuster le traitement si nécessaire. La kinésithérapie et les programmes d'exercices à long terme sont essentiels pour préserver la santé de la colonne vertébrale et prévenir les complications.
Soutien et ressources pour les personnes atteintes de scoliose à cage thoracique irrégulière
Vivre avec une scoliose à cage thoracique irrégulière peut être difficile, tant sur le plan physique qu'émotionnel. Les groupes de soutien, les ressources éducatives et les organisations de défense des droits fournissent des informations essentielles et un soutien émotionnel. Le contact avec d'autres personnes partageant des expériences similaires peut s'avérer inestimable pour naviguer dans les complexités de la maladie.
Conclusion
La scoliose à cage thoracique irrégulière est une affection complexe qui nécessite une prise en charge globale. Une détection précoce et une intervention rapide sont essentielles pour minimiser l'impact sur le bien-être physique et psychologique. Les traitements non chirurgicaux, tels que la kinésithérapie et les attelles, sont efficaces dans de nombreux cas, tandis que les options chirurgicales restent possibles dans les cas graves. Avec des soins et un soutien continus, les personnes atteintes de scoliose à cage thoracique irrégulière peuvent mener une vie épanouie.
Références
- Trobisch P, Suess O, Schwab F. "Scoliose idiopathique". Dtsch Arztebl Int. 2010;107(49):875-883. doi : 10.3238/arztebl.2010.0875.
- Weinstein SL, Dolan LA, Cheng JC, Danielsson A, Morcuende JA. "Scoliose idiopathique de l'adolescent". Lancet. 2008;371(9623):1527-1537. doi : 10.1016/S0140-6736(08)60658-3.
- Kaspiris A, Grivas TB, Weiss HR, Turnbull D. "Scoliosis : Examen du diagnostic et du traitement". Journal international d'orthopédie. 2013;37(1):34-42. doi : 10.1038/s41390-020-1047-9.
- Miller NH. "Cause et histoire naturelle de la scoliose idiopathique de l'adolescent". Orthop Clin North Am. 1999;30(3):343-352. doi : 10.1016/S0030-5898(05)70093-0.
- Hedequist DJ, Emans JB. "Scoliose congénitale : A review and update". J Pediatr Orthop. 2007;27(1):106-116. doi : 10.1097/01.bpo.0000248569.45965.79.
- Bowen JR, Newton PO, Mahar AT. "Scoliose neuromusculaire : Treatment and management". Journal des troubles et techniques de la colonne vertébrale. 2001;14(4):283-293. doi : 10.1097/00002517-200108000-00001.
- Ploumis A, Transfledt EE, Denis F. "Scoliose lombaire dégénérative associée à une sténose spinale". Dos J. 2007;7(4):428-436. doi : 10.1016/j.spinee.2006.07.017.
- Negrini S, Donzelli S, Aulisa AG, et al. "2016 SOSORT guidelines : Traitement orthopédique et de rééducation de la scoliose idiopathique pendant la croissance." Scoliose et troubles de la colonne vertébrale. 2018;13:3. doi : 10.1186/s13013-018-0175-8.
- Lonstein JE, Carlson JM. "The prediction of curve progression in untreated idiopathic scoliosis during growth" (La prédiction de la progression de la courbe dans la scoliose idiopathique non traitée pendant la croissance). J Bone Joint Surg Am. 1984;66(7):1061-1071. doi : 10.2106/00004623-198466070-00008.
- Danielsson AJ, Nachemson AL. "Douleurs dorsales et fonction 23 ans après l'arthrodèse pour la scoliose idiopathique de l'adolescent : A case-control study-Part II". Spine (Phila Pa 1976). 2003;28(18). doi : 10.1097/01.BRS.0000083720.30869.0D.
- Monticone M, Ambrosini E, Cazzaniga D, Rocca B, Ferrante S. "Active self-correction and task-oriented exercises reduce spinal deformity and improve quality of life in subjects with mild adolescent idiopathic scoliosis : Results of a randomized controlled trial". Eur Spine J. 2016;25(10):3118-3127. doi : 10.1007/s00586-016-4625-4.
- Negrini S, Hresko TM, O'Brien JP, et al. "Recommandations pour les études de recherche sur le traitement de la scoliose idiopathique". Scoliose et troubles de la colonne vertébrale. 2016;11:28. doi : 10.1186/s13013-016-0084-9.
- Kotwicki T, Negrini S, Grivas TB, et al. "Methodology of evaluation of scoliosis, back deformities and posture". Scoliose. 2009;4:26. doi : 10.1186/1748-7161-4-26.
- Bettany-Saltikov J, Weiss HR, Chockalingam N, et al. "Surgical versus non-surgical interventions in people with adolescent idiopathic scoliosis". Cochrane Database Syst Rev. 2015;2015(4). doi : 10.1002/14651858.CD010663.pub2.
- Kaspiris A, Grivas TB, Weiss HR. "Prise en charge des patients atteints de scoliose". Eur J Phys Rehabil Med. 2014;50(2):111-120. doi : 10.23736/S1973-9087.14.03344-2.