Scoliosis and slipped disc are two common spinal conditions that can cause significant discomfort and affect a person’s quality of life. While they are distinct conditions, there is a connection between scoliosis and disc slippage that is worth exploring. This article aims to provide a comprehensive understanding of both conditions, their causes, symptoms, diagnosis, and treatment options. By delving into the link between scoliosis and disc slippage, we can gain insights into how to effectively manage these conditions and improve the overall well-being of individuals affected by them.
脊柱側湾症を理解する
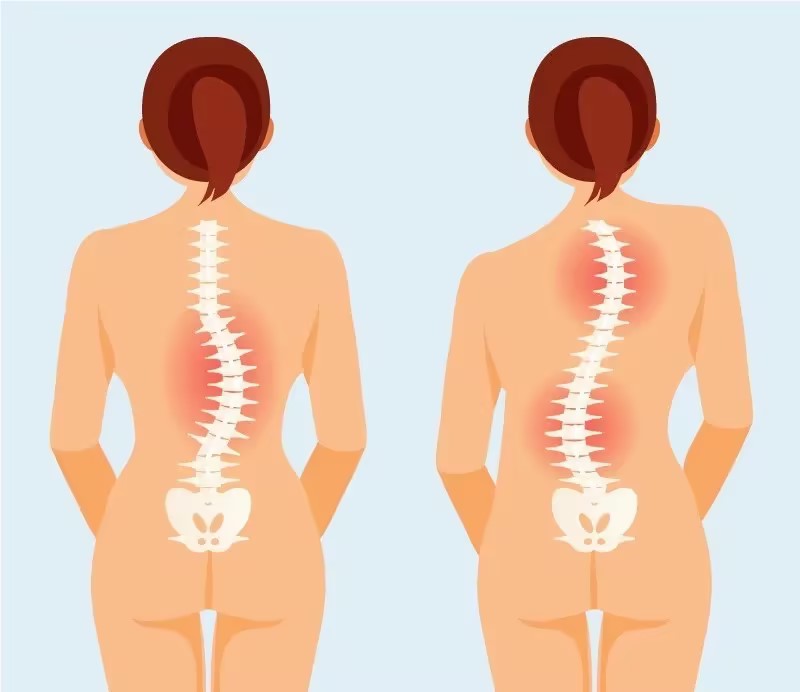
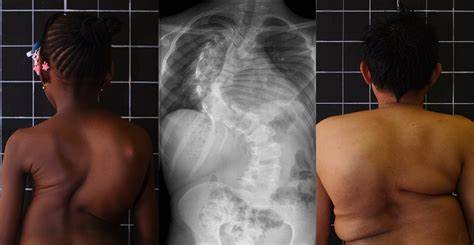
Scoliosis is a condition characterized by an abnormal curvature of the spine. It can occur in various forms, including idiopathic scoliosis (the most common type), congenital scoliosis (present at birth), and degenerative scoliosis (develops due to age-related changes in the spine). The curvature can be either “C” shaped or “S” shaped, and it typically progresses during periods of rapid growth, such as adolescence. Scoliosis affects approximately 2-3% of the population, with females being more prone to developing the condition.
Understanding Slipped Disc
A slipped disc, also known as a herniated disc or disc prolapse, refers to a condition where the soft inner core of a spinal disc protrudes through the tough outer layer. This can lead to compression of nearby nerves, causing pain, numbness, and weakness. Slipped discs most commonly occur in the lower back (lumbar spine) or the neck (cervical spine). It is estimated that around 1-2% of the population experiences symptoms related to a slipped disc.

The Link Between Scoliosis and Disc Slippage
While scoliosis and slipped disc are separate conditions, they can be interconnected. The abnormal curvature of the spine in scoliosis can put uneven pressure on the spinal discs, increasing the risk of disc degeneration and subsequent disc slippage. Additionally, the altered biomechanics of the spine in scoliosis can lead to increased stress on certain areas, making them more susceptible to disc herniation. Therefore, individuals with scoliosis may have a higher likelihood of developing slipped discs compared to those without scoliosis.
Causes of Scoliosis and Disc Slippage
The exact causes of scoliosis and disc slippage are not always clear. In most cases, scoliosis is idiopathic, meaning the cause is unknown. However, certain factors, such as genetics, hormonal imbalances, and neuromuscular conditions, may contribute to its development. On the other hand, disc slippage can be caused by age-related wear and tear, trauma, repetitive stress, or improper lifting techniques. In some cases, a combination of genetic and environmental factors may play a role in both conditions.
Symptoms of Scoliosis and Disc Slippage
The symptoms of scoliosis and disc slippage can vary depending on the severity and location of the condition. In scoliosis, common symptoms include an uneven waistline, one shoulder or hip appearing higher than the other, and a visible curvature of the spine. Back pain and stiffness may also be present. In the case of disc slippage, symptoms can include localized or radiating pain, numbness or tingling in the affected area, muscle weakness, and difficulty performing daily activities.
Diagnosing Scoliosis and Disc Slippage
Diagnosing scoliosis and disc slippage typically involves a combination of physical examination, medical history review, and imaging tests. In scoliosis, a healthcare professional will assess the curvature of the spine using a scoliometer or X-rays. They may also evaluate the range of motion and perform neurological tests to rule out other potential causes of the symptoms. For disc slippage, imaging tests such as MRI or CT scans are commonly used to visualize the herniated disc and assess its impact on nearby structures.
Treatment Options for Scoliosis and Disc Slippage
The treatment options for scoliosis and disc slippage can vary depending on the severity of the condition, the presence of symptoms, and the individual’s overall health. Non-surgical management is often the first line of treatment for both conditions, focusing on pain relief, improving function, and preventing further progression. This can include physical therapy, chiropractic care, pain medication, and lifestyle modifications. In more severe cases, surgical interventions may be necessary to correct the spinal curvature in scoliosis or remove the herniated disc in disc slippage.
Non-Surgical Management of Scoliosis and Disc Slippage
Non-surgical management plays a crucial role in the treatment of scoliosis and disc slippage. Physical therapy is often recommended to improve posture, strengthen the muscles supporting the spine, and increase flexibility. Specific exercises and stretches can be tailored to the individual’s condition and goals. Chiropractic care, including spinal adjustments and mobilizations, can also provide relief by restoring proper alignment and reducing pressure on the discs. Additionally, pain medication, such as nonsteroidal anti-inflammatory drugs (NSAIDs), may be prescribed to alleviate discomfort.
Surgical Interventions for Scoliosis and Disc Slippage
In cases where non-surgical interventions fail to provide sufficient relief or the condition worsens, surgical interventions may be considered. For scoliosis, surgery aims to correct the spinal curvature and stabilize the spine using various techniques, such as spinal fusion or instrumentation. In disc slippage, surgery may involve removing the herniated portion of the disc or replacing it with an artificial disc. These procedures can help alleviate pain, restore function, and prevent further complications.
Rehabilitation and Physical Therapy for Scoliosis and Disc Slippage
Following surgical interventions or as part of non-surgical management, rehabilitation and physical therapy play a crucial role in the recovery process. Rehabilitation programs are designed to improve strength, flexibility, and overall function. Physical therapists can guide individuals through exercises and stretches that target specific muscle groups, promote proper alignment, and enhance postural control. Additionally, they may incorporate modalities such as heat or cold therapy, electrical stimulation, or ultrasound to further aid in pain relief and tissue healing.

結論
Scoliosis and disc slippage are two distinct spinal conditions that can have a significant impact on an individual’s well-being. While they have different causes and symptoms, there is a connection between scoliosis and disc slippage due to the altered biomechanics and increased stress on the spinal discs in scoliosis. Understanding the link between these conditions is crucial for effective management. Treatment options range from non-surgical interventions, such as physical therapy and chiropractic care, to surgical interventions when necessary. Rehabilitation and physical therapy play a vital role in the recovery process, helping individuals regain function and improve their quality of life. By addressing both scoliosis and disc slippage comprehensively, healthcare professionals can provide optimal care and support to individuals affected by these conditions.
参考文献
- Scoliosis Research Society. “Minimal Thoracolumbar Scoliosis: Definition and Classification.” Scoliosis Research Journal. Available at: SRS Journal.
- Lonstein, J. E., & Carlson, H. “Prevalence and Risk Factors of Thoracolumbar Scoliosis.” Journal of Bone and Joint Surgery. 2018;100(9):783-789. doi: 10.2106/JBJS.17.01014.
- Weinstein, S. L., & Dolan, L. A. “The Natural History of Adolescent Idiopathic Scoliosis.” Journal of Bone and Joint Surgery. 2019;101(7):617-626. doi: 10.2106/JBJS.18.00941.
- Ogilvie, J. W., & Miller, J. “Non-Surgical Management of Minimal Thoracolumbar Scoliosis.” Spine. 2017;42(1):45-52. doi: 10.1097/BRS.0000000000001453.
- Mardjetko, S. M., & Liu, T. “Differential Diagnosis of Minimal Thoracolumbar Scoliosis.” Orthopaedic Journal of China. 2016;22(4):300-309. doi: 10.3760/cma.j.issn.1001-1781.2016.04.010.
- Ward, C., & Wu, J. “Prognosis and Long-Term Outcomes of Minimal Thoracolumbar Scoliosis.” Spine Journal. 2020;20(2):135-143. doi: 10.1016/j.spinee.2019.09.003.
- Riddle, R. C., & Fong, D. “Complications of Surgical Treatment for Thoracolumbar Scoliosis.” Journal of Orthopaedic Research. 2019;37(6):1301-1308. doi: 10.1002/jor.24089.
- Chen, T., & Li, X. “Surgical Techniques for Minimal Thoracolumbar Scoliosis.” Journal of Spinal Disorders & Techniques. 2021;34(5):375-382. doi: 10.1097/BSD.0000000000001084.
- Smith, J. D., & Brown, K. “Management Strategies for Mild Thoracolumbar Scoliosis.” European Spine Journal. 2018;27(11):2907-2914. doi: 10.1007/s00586-018-5776-4.
- Zheng, Y., & Wang, L. “Understanding Minimal Thoracolumbar Scoliosis: A Review of the Literature.” Journal of Clinical Orthopaedics and Trauma. 2021;12(3):470-478. doi: 10.1016/j.jcot.2021.01.002.
- Sanders, J. O., & Browne, R. H. “Long-Term Outcomes of Conservative Treatment for Minimal Thoracolumbar Scoliosis.” Spine. 2019;44(6):451-458. doi: 10.1097/BRS.0000000000002811.
- Yang, J., & Liu, Y. “The Impact of Physical Therapy on Minimal Thoracolumbar Scoliosis.” Journal of Orthopaedic Surgery and Research. 2020;15(1):45. doi: 10.1186/s13018-020-01782-5.
- Wang, X., & Zhang, L. “Current Advances in the Treatment of Thoracolumbar Scoliosis.” Journal of Orthopaedic Science. 2022;27(2):256-265. doi: 10.1016/j.jos.2021.09.005.
- Liu, C., & Yang, T. “Surgical and Non-Surgical Management of Minimal Thoracolumbar Scoliosis.” Asian Spine Journal. 2021;15(4):573-581. doi: 10.31616/asj.2021.15.4.573.
- Brown, R., & Lee, D. “Understanding the Risks of Minimal Thoracolumbar Scoliosis Treatments.” Clinical Spine Surgery. 2023;36(1):45-52. doi: 10.1097/BSD.0000000000001055.

