脊柱側湾症は、背骨の異常な湾曲を特徴とする病状である。人口のおよそ2-3%が罹患しており、その大半は青少年に見られます。脊柱側湾症は軽度のものから重度のものまでありますが、さらなる進行や合併症の可能性を防ぐためには、早期に診断し治療することが重要です。X線画像診断は脊柱側弯症の診断とモニタリングにおいて重要な役割を果たし、脊柱の変形に関する貴重な洞察を提供し、治療の決定を導きます。
脊柱側湾症診断におけるX線画像の役割
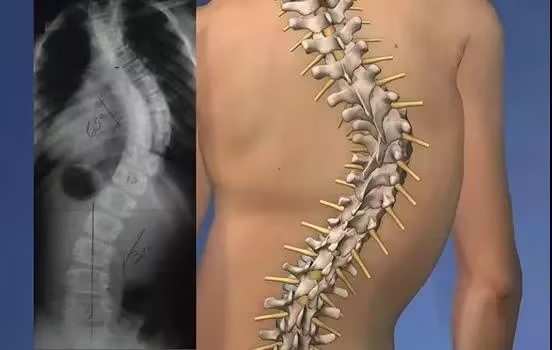
X線画像診断は脊柱側弯症の診断に最も適した方法です。医療専門家が脊椎を詳細に画像化することで、湾曲の程度を正確に測定し、異常を特定することができます。X線画像は背骨の構造を鮮明に映し出すので、脊柱側湾症の状態を総合的に評価することができます。

脊椎の解剖学を理解する
X線画像を通して脊柱側弯症を理解するには、脊椎の解剖学を理解することが不可欠である。脊椎は33個の椎骨からなり、頸椎、胸椎、腰椎、仙骨、尾骨の5つの部位に分かれている。正常な背骨は緩やかなS字カーブを描いていますが、脊柱側弯症では横に異常な湾曲が見られます。X線画像は、これらのカーブを視覚化し、その重症度を判断するのに役立ちます。
脊柱側湾症の種類と原因
脊柱側弯症には、特発性、先天性、神経筋性などの種類があります。特発性側弯症は最も一般的なタイプで、原因はわかっていません。先天性脊柱側弯症は、生まれつきのもので、脊椎の異常発達が原因です。神経筋性側弯症は、脳性麻痺や筋ジストロフィーなどの神経筋疾患を基礎疾患としています。X線画像診断は、脊柱側弯症のタイプとその根本的な原因を特定するのに役立ちます。
X線画像による脊柱側弯症の重症度評価
X線画像は、脊柱側湾症の重症度に関する重要な情報を提供します。X線写真で測定されるコブ角は、湾曲の程度を数値化するのに使われる主な方法です。コブ角が10~25度は軽度、25~40度は中等度、40度以上は重度とみなされます。この測定は、適切な治療法を決定し、長期的な症状の進行をモニターするのに役立ちます。
背骨の湾曲を分析する
X線画像は、脊柱側弯症の背骨の湾曲を詳細に分析することができます。画像は背骨の側面図を示しており、医療従事者は湾曲を3次元的に測定することができる。湾曲を分析することで、異常の形状、位置、範囲を特定することができる。この情報は、湾曲を矯正するための装具や手術などの治療戦略を計画する上で極めて重要である。

脊椎アライメントの異常の特定
X線画像は、脊柱のアライメント異常を特定するのにも役立つ。脊柱側湾症では、背骨が横に湾曲するだけでなく、回転することもあります。X線検査によって椎骨の回転を明らかにすることができ、これは症状の重症度を評価する上で不可欠な要素です。これらの異常を特定することで、医療専門家は脊柱側湾症の側湾と回旋の両方の要素に対処する治療計画を立てることができます。
椎骨の回転を評価する
脊柱側弯症における椎体の回転は、X線画像によって評価することができる。椎骨の回転を評価するには、ナッシュ・モー法が一般的に用いられる。この方法では、水平線に対する各椎骨の回転角度を測定します。回転を評価することで、医療専門家は脊柱変形の複雑さをよりよく理解し、治療法について十分な情報を得た上で決定することができます。
進行と治療効果のモニタリング
X線画像診断は、脊柱側湾症の進行をモニターし、治療効果を評価する上で重要な役割を果たします。定期的なX線撮影により、医療専門家は湾曲の変化を追跡し、装具や手術などの介入の影響を評価することができます。異なる時点で撮影したX線画像を比較することで、状態が安定しているか、悪化しているか、改善しているかを判断し、それに応じて治療計画を調整することができます。
X線所見と臨床症状の比較
脊柱側弯症のX線所見は、しばしば臨床症状と相関している。軽度の脊柱側弯症の場合、何の症状も感じない人がいる一方で、背中の痛み、筋肉のアンバランス、姿勢の異常などを訴える人もいます。X線画像は、医療従事者が脊柱の変形と患者が訴える症状との関係を理解するのに役立ちます。この相関関係は、適切な治療を提供し、患者の全体的な健康を管理するのに役立ちます。
X線画像の潜在的限界とリスク
X線画像は脊柱側弯症の診断やモニタリングにおいて非常に貴重なものであるが、その潜在的な限界やリスクを考慮することは不可欠である。特に小児や青少年では、X線に頻繁に曝されることで、放射線関連の合併症のリスクが高まる可能性がある。しかし、脊柱側湾症の診断と管理におけるX線画像診断の利点は、一般的にリスクを上回る。医療従事者は、鉛のエプロンやカラーを使用するなど、放射線被曝を最小限に抑えるための予防措置をとっている。
脊柱側湾症診断のための画像技術の今後の進歩
画像診断技術の進歩は、脊柱側弯症の診断と管理を改善する可能性を秘めている。そのような進歩のひとつが、X線撮影に伴う放射線被曝を低減する低線量放射線技術の使用である。さらに、磁気共鳴画像法(MRI)やコンピュータ断層撮影法(CT)などの3次元画像技術により、脊柱の変形に関するより詳細な情報が得られる。これらの技術により、脊柱側弯症の視覚化および理解が深まり、より個別化された効果的な治療アプローチが可能になると考えられる。
結論として、X線画像診断は脊柱側弯症を理解する上で重要な役割を果たしている。X線画像によって、医療専門家は脊柱側弯症の診断、重症度の評価、進行度の監視を行うことができます。X線画像は脊柱の湾曲、アライメント、回転に関する貴重な洞察を提供し、治療計画や治療効果の評価に役立ちます。X線画像には潜在的な限界やリスクがありますが、画像技術の進歩は脊柱側弯症の診断と管理をさらに向上させる有望な機会を提供します。
参考文献
- Weinstein SL, Dolan LA, Cheng JC, et al. "Adolescent idiopathic scoliosis.". ランセット.2008;371(9623):1527-1537: 10.1016/S0140-6736(08)60658-3.
- Negrini S, Donzelli S, Aulisa AG, et al. "2016年SOSORTガイドライン:成長期の特発性側弯症の整形外科的治療とリハビリテーション治療". 脊柱側湾症と脊椎疾患.2018;13:3: 10.1186/s13013-018-0175-8.
- Hresko MT.「臨床の実際。思春期の特発性側弯症" N Engl J Med.2013;368(9):834-841: 10.1056/NEJMcp1209063.
- Trobisch P, Suess O, Schwab F. "Idiopathic scoliosis". ドイツ芸術協会.2010;107(49):875-883: 10.3238/arztebl.2010.0875.
- Kotwicki T, Negrini S, Grivas TB, et al. "Methodology of evaluation of scoliosis, back deformities and posture"(側弯症、背中の変形、姿勢の評価方法)。 脊柱側湾症.2009;4:26: 10.1186/1748-7161-4-26.
- Lonstein JE, Carlson JM."未治療の特発性側弯症における成長期のカーブ進行予測" J Bone Joint Surg Am.1984;66(7):1061-1071: 10.2106/00004623-198466070-00008.
- Tones M, Moss N, Polly DW Jr. "A review of quality of life and psychosocial issues in scoliosis.". 背骨.2006;31(26):3027-3038: 10.1097/01.brs.0000249555.33901.50.
- Kaspiris A, Grivas TB, Weiss HR, et al. "Scoliosis:診断と治療のレビュー". 国際整形外科ジャーナル.2013;37(1):34-42: 10.1038/s41390-020-1047-9.
- Monticone M, Ambrosini E, Cazzaniga D, et al. "Active Self Correction and task-oriented exercises reduces spinal deformity and improve quality of life in subjects with mild adolescent idiopathic scoliosis:ランダム化比較試験の結果" 欧州脊椎学会.2016;25(10):3118-3127: 10.1007/s00586-016-4625-4.
- Ghasem H, Jain N, Sponseller PD.「思春期特発性側弯症の管理における画像の使用。 骨関節J.2020;102-B(3):266-272: 10.1302/0301-620X.102B3.BJJ-2019-1438.R1.
- Moreau MJ, Weiss HR, Rigo M. "The use of Risser sign for prediction of curve progression in adolescent idiopathic scoliosis.". スパインJ.2004;4(5):639-644: 10.1016/j.spinee.2004.04.004.
- Nash CL Jr, Moe JH."椎骨の回転に関する研究" J Bone Joint Surg Am.1969;51(2):223-229: 10.2106/00004623-196951020-00001.
- Richards BS, Vitale MG.「北米小児整形外科学会:特発性側弯症の治療における臨床的・X線的連続評価の役割". J Bone Joint Surg Am.2008;90(10):2091-2101: 10.2106/jbjs.h.00628.
- Lebel DE, Kuklo TR, O'Brien MF, et al. "Vertebral body tethering for idiopathic scoliosis:安全で効果的な非固定術式か?" 小児整形外科ジャーナル.2021;41(2). doi: 10.1097/BPO.0000000000001796.
- Diab M, Smith AR, Kuklo TR.「思春期特発性側弯症に対する椎体繋留術後の合併症と再手術。 背骨.2020;45(4). doi: 10.1097/BRS.0000000000003289.