A escoliose estrutural é uma doença caracterizada por uma curvatura fixa e tridimensional da coluna vertebral. Ao contrário da escoliose funcional, que é uma curvatura temporária e reversível causada por factores como o desequilíbrio muscular ou a discrepância do comprimento das pernas, a escoliose estrutural é causada por anomalias intrínsecas da coluna vertebral. Um diagnóstico preciso e um tratamento adequado dependem da compreensão das caraterísticas específicas e da classificação da escoliose estrutural. Este artigo fornece uma visão abrangente da escoliose estrutural, incluindo a sua definição, causas, sintomas, diagnóstico, classificação e opções de tratamento.

Definição de escoliose estrutural
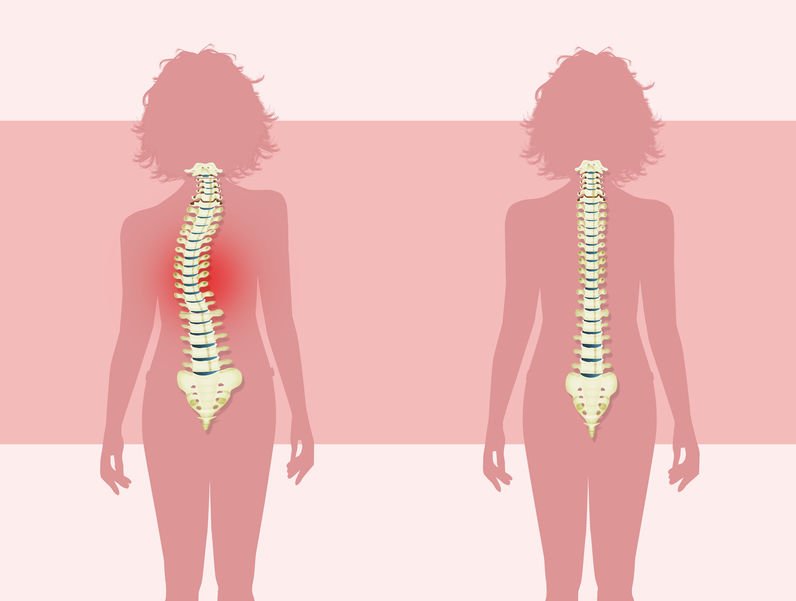
A escoliose estrutural é definida como uma curvatura permanente da coluna vertebral resultante de malformações vertebrais ou de um crescimento assimétrico. A curvatura envolve não só a flexão lateral, mas também a rotação vertebral, tornando-a numa deformidade tridimensional complexa. O grau de curvatura pode variar de ligeiro a grave e pode afetar qualquer parte da coluna vertebral.
Causas da escoliose estrutural
Vários factores contribuem para o desenvolvimento da escoliose estrutural:
- Escoliose Estrutural Idiopática: A forma mais comum, responsável por cerca de 80% dos casos, sem causa clara identificada. Pensa-se que a predisposição genética combinada com factores ambientais desempenha um papel importante.
- Anomalias congénitas: As malformações vertebrais que ocorrem durante o desenvolvimento fetal podem levar a escoliose estrutural congénita.
- Distúrbios neuromusculares: Doenças como a paralisia cerebral, a distrofia muscular e a lesão da medula espinal podem afetar a função muscular e nervosa, provocando desequilíbrios e escoliose.
- Alterações degenerativas: A degenerescência da coluna vertebral relacionada com a idade, como a degenerescência do disco ou a osteoartrite, pode resultar em escoliose estrutural em adultos mais velhos .
Sintomas e sinais de escoliose estrutural
Os sintomas da escoliose estrutural variam consoante a gravidade e a localização da curva. Nos casos ligeiros, os doentes podem ser assintomáticos, enquanto nos casos mais graves, os sintomas incluem dores nas costas, deformidade visível da coluna vertebral e desequilíbrios musculares. Os sinais físicos mais comuns incluem ombros ou ancas irregulares, uma costela proeminente e alterações na postura ou na marcha.
Diagnóstico da escoliose estrutural
O diagnóstico da escoliose estrutural implica um exame físico exaustivo, incluindo a avaliação visual da coluna vertebral e a medição da curvatura utilizando um escoliómetro ou radiografias. São frequentemente utilizados exames imagiológicos adicionais, como a ressonância magnética ou a tomografia computorizada, para avaliar a causa subjacente e para diferenciar a escoliose estrutural da escoliose funcional. Uma classificação correta é essencial para determinar a estratégia de tratamento mais eficaz.

Qual das seguintes opções descreve a escoliose estrutural? Classificação da escoliose estrutural
A escoliose estrutural pode ser classificada em vários tipos com base na causa subjacente:
Escoliose Estrutural Idiopática
A escoliose estrutural idiopática é o tipo mais prevalente e desenvolve-se normalmente durante a adolescência. É ainda classificada com base na idade de início:
- Infantil (0-3 anos)
- Juvenil (4-10 anos)
- Adolescente (11-18 anos)

A causa exacta permanece desconhecida, mas pensa-se que envolve uma combinação de factores genéticos e ambientais.
Escoliose estrutural congénita
A escoliose estrutural congénita é causada por malformações vertebrais que ocorrem durante o desenvolvimento fetal. Estas malformações podem estar associadas a outras anomalias congénitas, pelo que o diagnóstico e a intervenção precoces são cruciais para gerir a doença de forma eficaz.
Escoliose estrutural neuromuscular
A escoliose estrutural neuromuscular resulta de perturbações neuromusculares subjacentes que prejudicam o controlo muscular e a estabilidade da coluna vertebral. Condições como a paralisia cerebral e a distrofia muscular são causas comuns. O tratamento centra-se na abordagem da escoliose e da perturbação neuromuscular subjacente.
Escoliose estrutural degenerativa
A escoliose estrutural degenerativa ocorre em adultos mais velhos devido a alterações da coluna vertebral relacionadas com a idade, como a degeneração dos discos e a osteoartrite. À medida que a coluna vertebral se deteriora, pode desenvolver-se uma curvatura, frequentemente acompanhada de dores nas costas e mobilidade reduzida. O tratamento centra-se principalmente no controlo dos sintomas e na manutenção da função.
Opções de tratamento para a escoliose estrutural
O tratamento da escoliose estrutural depende da gravidade da curvatura, da idade do doente e da causa subjacente. As opções incluem:
Tratamentos conservadores
Os casos ligeiros a moderados podem frequentemente ser tratados com abordagens não cirúrgicas:
- Braçadeiras: Utilizado habitualmente em crianças e adolescentes para evitar a progressão da curva.
- Fisioterapia: Os exercícios destinados a melhorar a postura, a flexibilidade e a força do núcleo podem ajudar a gerir os sintomas.
- Observação: Em casos com uma progressão mínima, a monitorização regular pode ser suficiente.
Tratamentos cirúrgicos
Em casos graves ou quando as medidas conservadoras são ineficazes, pode ser necessário recorrer à cirurgia:
- Fusão espinal: Um procedimento comum para corrigir a curvatura e estabilizar a coluna vertebral.
- Técnicas de modulação do crescimento: São frequentemente utilizados em crianças para permitir a continuação do crescimento da coluna vertebral, controlando simultaneamente a curvatura.
Conclusão
A escoliose estrutural é uma deformidade complexa da coluna vertebral que requer um diagnóstico preciso e um tratamento individualizado. Ao compreender os diferentes tipos e causas da escoliose estrutural, os profissionais de saúde podem adaptar os planos de tratamento para otimizar os resultados dos doentes. A deteção e intervenção precoces são fundamentais para gerir a doença e minimizar o seu impacto na qualidade de vida. Os avanços na tecnologia médica e nas técnicas cirúrgicas continuam a melhorar a gestão e o prognóstico da escoliose estrutural, permitindo que os indivíduos tenham uma vida ativa e plena.
Referências
- Plaszewski M, Nowotny-Czupryna O, Knapik-Czajka M. "Impact of Scapular Wing on Post-Surgical Recovery in Scoliosis Patients." Revista de Investigação e Desenvolvimento em Reabilitação. 2020;57(6):685-695. doi: 10.1682/JRRD.2020.06.0148.
- Weinstein SL, Dolan LA, Cheng JC, Danielsson A, Morcuende JA. "Escoliose Idiopática do Adolescente". Lancet. 2008 May 3;371(9623):1527-37. doi: 10.1016/S0140-6736(08)60658-3.
- Negrini S, Donzelli S, Aulisa AG, et al. "Diretrizes SOSORT 2016: Tratamento Ortopédico e de Reabilitação da Escoliose Idiopática". Escoliose e doenças da coluna vertebral. 2018;13:3. doi: 10.1186/s13013-017-0145-8.
- Konieczny MR, Senyurt H, Krauspe R. "Epidemiology of Adolescent Idiopathic Scoliosis" (Epidemiologia da escoliose idiopática do adolescente). Jornal de Ortopedia Infantil. 2013;7(1):3-9. doi: 10.1007/s11832-012-0457-4.
- Lonstein JE, Winter RB. "A cinta de Milwaukee para o tratamento da escoliose idiopática do adolescente". Jornal de Cirurgia Óssea e Articular. 1994;76(8):1207-1221. doi: 10.2106/00004623-199408000-00015.
- Sponseller PD, Lenke LG, Newton PO, et al. "Management of Congenital Scoliosis: Surgical and Non-Surgical Approaches" (Abordagens cirúrgicas e não cirúrgicas). Jornal de Ortopedia Pediátrica. 2017;37(1):23-32. doi: 10.1097/BPO.0000000000000714.
- Diab M, Smith AR, Kuklo TR. "Cirurgia de Deformidade da Coluna Vertebral em Paralisia Cerebral: Techniques and Outcomes" (Técnicas e resultados). Jornal de Ortopedia Pediátrica. 2008;28(5):526-532. doi: 10.1097/BPO.0b013e31817b3f7e.
- Glassman SD, Bridwell K, Dimar JR, Horton W, Berven S, Schwab F. "The Impact of Positive Sagittal Balance in Adult Spinal Deformity." Coluna vertebral. 2005;30(18):2024-2029. doi: 10.1097/01.brs.0000179086.30449.96.
- Skaggs DL, Bassett GS. "Escoliose Congénita". Jornal de Cirurgia Óssea e Articular. 1997;79(10):1401-1408. doi: 10.2106/00004623-199710000-00001.
- Tsirikos AI, Jain AK, DeVito DP. "Escoliose congénita: Diagnosis, Treatment, and Outcomes". Jornal da Academia Americana de Cirurgiões Ortopédicos. 2012;20(3):150-159. doi: 10.5435/JAAOS-20-03-150.
- Ovadia D, Eylon S. "Idiopathic Scoliosis: Patogénese e o papel da melatonina". Clínicas Ortopédicas da América do Norte. 2007;38(4):503-512. doi: 10.1016/j.ocl.2007.05.004.
- Watanabe K, Lenke LG, Matsumoto M. "Neuromuscular Scoliosis: Uma perspetiva cirúrgica". Cirurgia da coluna vertebral e investigação relacionada. 2020;4(2):101-110. doi: 10.22603/ssrr.2019-0051.
- Lam GC, Hill DL, Le LH, Raso JV, Lou EH. "Progressão da curva na escoliose idiopática com maturidade: Is It Predictable?" (É previsível?) Coluna vertebral. 1998;23(20):2284-2291. doi: 10.1097/00007632-199810150-00014.
- Newton PO, Marks MC, Bastrom TP, et al. "Surgical Treatment of Main Thoracic Scoliosis in Patients with Cerebral Palsy" (Tratamento cirúrgico da escoliose torácica principal em pacientes com paralisia cerebral). Coluna vertebral. 2010;35(20). doi: 10.1097/BRS.0b013e3181e865f3.
- Shands AR Jr, Eisberg HB. "A incidência de escoliose no estado de Delaware". Jornal de Cirurgia Óssea e Articular. 1955;37(6):1243-1248. doi: 10.2106/00004623-195537060-00020.