Scoliosis is a condition characterized by an abnormal curvature of the spine, which can lead to various physical and functional impairments. To accurately diagnose and assess the severity of scoliosis, a comprehensive physical examination is essential. This examination involves a series of assessments and tests that provide valuable information about the condition, its impact on daily life, and the appropriate treatment options.
Preparing for the Examination
Before undergoing a scoliosis physical examination, it is important to prepare adequately. This includes wearing loose-fitting clothing that allows for easy movement and access to the spine. Additionally, it is advisable to bring any relevant medical records, such as previous X-rays or MRI scans, to provide a comprehensive overview of the condition.
Initial Assessment and Medical History
The scoliosis physical examination typically begins with an initial assessment and medical history review. The healthcare provider will inquire about any symptoms, such as back pain or difficulty breathing, as well as any previous treatments or surgeries related to scoliosis. This information helps establish a baseline understanding of the condition and guides further examination.
Visual Inspection and Postural Assessment
Visual inspection and postural assessment are crucial components of the scoliosis physical examination. The healthcare provider will observe the patient’s standing posture from various angles, looking for any signs of asymmetry, such as uneven shoulders or hips, a tilted pelvis, or a noticeable curvature of the spine. These visual cues provide valuable insights into the presence and severity of scoliosis.
Range of Motion Testing
Range of motion testing is performed to assess the flexibility and mobility of the spine. The patient will be asked to perform various movements, such as bending forward, backward, and to the sides. The healthcare provider will carefully observe the range of motion and note any limitations or discomfort experienced by the patient. Restricted range of motion can indicate the presence of scoliosis and help determine the appropriate treatment approach.
Neurological Examination
A neurological examination is an essential part of the scoliosis physical examination. The healthcare provider will assess the patient’s reflexes, muscle strength, and sensation in the lower extremities. This examination helps identify any neurological abnormalities or nerve compression associated with severe scoliosis. It is particularly important in cases where surgical intervention may be necessary.
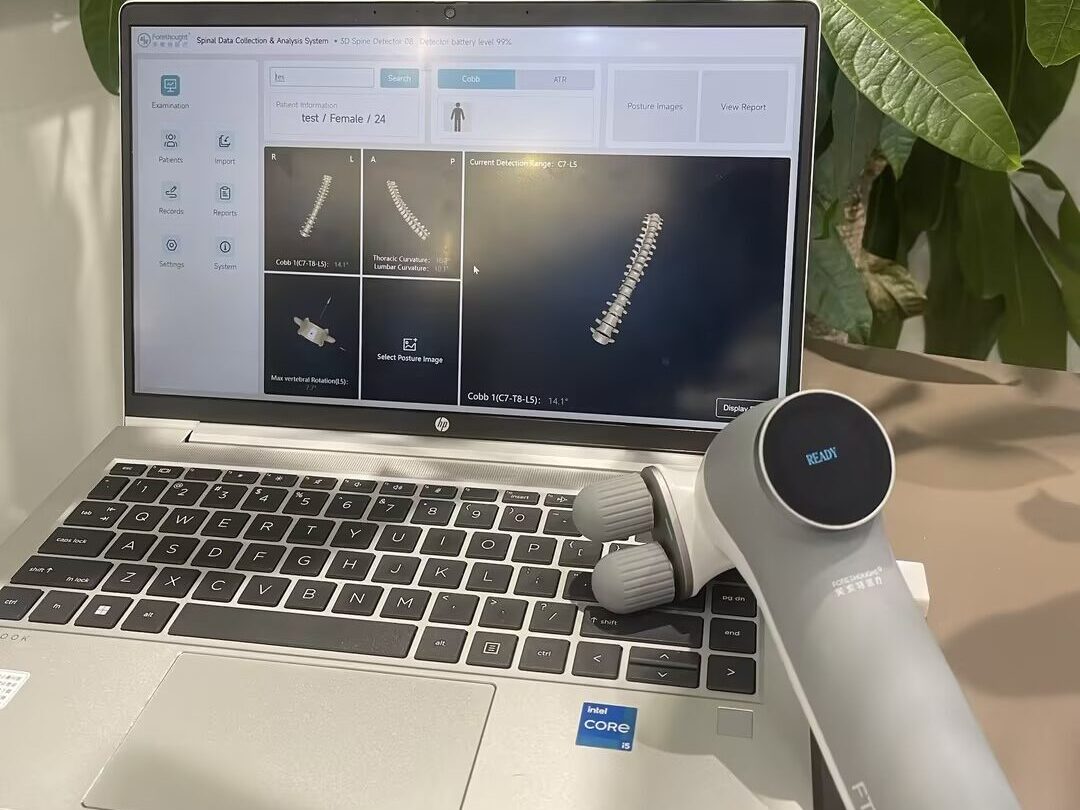
Radiographic Evaluation
Radiographic evaluation, including X-rays and sometimes MRI scans, is a critical component of the scoliosis physical examination. These imaging techniques provide detailed images of the spine, allowing for accurate measurement and assessment of the curvature. X-rays are commonly used to measure the Cobb angle, which quantifies the severity of the spinal curvature and guides treatment decisions.
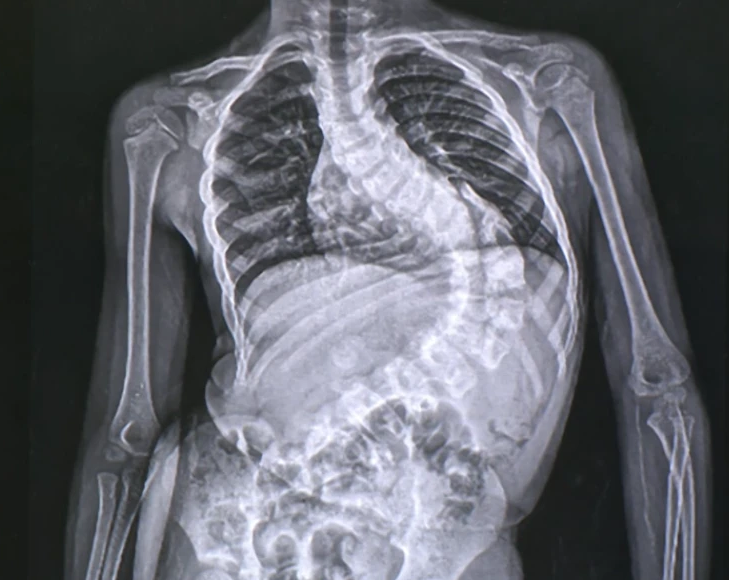
Cobb Angle Measurement
The Cobb angle measurement is a key parameter used to assess the severity of scoliosis. It is determined by measuring the angle between the upper and lower endplates of the most tilted vertebrae in the curve. A Cobb angle of less than 10 degrees is considered within the normal range, while angles greater than 10 degrees indicate the presence of scoliosis. The higher the Cobb angle, the more severe the curvature and the greater the impact on daily life.
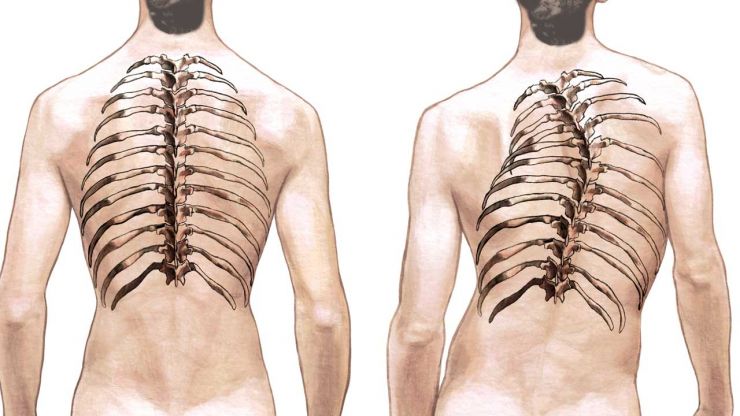
Assessing Rib Hump and Shoulder Asymmetry
During the scoliosis physical examination, the healthcare provider will assess for rib hump and shoulder asymmetry. Rib hump refers to the prominence of the ribs on one side of the spine, which can be visually observed when the patient bends forward. Shoulder asymmetry, on the other hand, refers to the uneven positioning of the shoulders. These assessments provide additional information about the severity and impact of scoliosis.
Evaluating Spinal Deformity Severity
The scoliosis physical examination also involves evaluating the severity of spinal deformity. This includes assessing the rotation of the vertebrae, the degree of lateral curvature, and the overall alignment of the spine. By carefully examining these factors, healthcare providers can determine the appropriate treatment options, such as bracing, physical therapy, or surgical intervention.
Functional Assessment and Impact on Daily Life
In addition to assessing the physical aspects of scoliosis, the examination also includes a functional assessment. This involves evaluating the impact of scoliosis on daily life activities, such as walking, sitting, and performing routine tasks. By understanding the functional limitations caused by scoliosis, healthcare providers can tailor treatment plans to address specific needs and improve overall quality of life.
Interpreting Examination Findings and Treatment Planning
Interpreting the findings of the scoliosis physical examination is crucial for developing an effective treatment plan. The healthcare provider will consider the severity of the curvature, the presence of any neurological abnormalities, the impact on daily life, and the patient’s age and overall health. Based on these factors, treatment options may include observation, bracing, physical therapy, or surgical intervention. The goal is to minimize the progression of the curvature, alleviate symptoms, and improve functional abilities.
In conclusion, the scoliosis physical examination is a comprehensive process that provides valuable insights into the severity and impact of scoliosis. Through visual inspection, range of motion testing, neurological examination, radiographic evaluation, and functional assessment, healthcare providers can accurately diagnose scoliosis, determine its severity, and develop appropriate treatment plans. By understanding the examination process and its significance, individuals with scoliosis can actively participate in their own care and achieve optimal outcomes.
References
- McCarthy I, McCarthy J. “The role of strength training in scoliosis management: a review.” Ther Adv Musculoskelet Dis. 2016;8(2):42-54. doi:10.1177/1759720X15619370. Available at: https://journals.sagepub.com/doi/10.1177/1759720X15619370
- Weinstein SL, Dolan LA, Cheng JC, et al. “Adolescent idiopathic scoliosis.” Lancet. 2008;371(9623):1527-1537. doi:10.1016/S0140-6736(08)60789-1. Available at: https://www.sciencedirect.com/science/article/pii/S0140673608607891
- McMaster MJ, Ogilvie JW. “The natural history of idiopathic scoliosis.” J Bone Joint Surg Am. 1982;64(5):712-717. doi:10.2106/00004623-198264050-00004. Available at: https://journals.lww.com/jbjsjournal/Abstract/1982/64050/THE_NATURAL_HISTORY_OF_IDIOPATHIC_SCOLIOSIS.4.aspx
- Kuru T, Yeldan İ, Dikici F, et al. “The effectiveness of exercise programs for idiopathic scoliosis.” Spine (Phila Pa 1976). 2008;33(10):1121-1128. doi:10.1097/BRS.0b013e31816cde1d. Available at: https://journals.lww.com/spinejournal/Abstract/2008/05150/The_Effectiveness_of_Exercise_Programs_for.9.aspx
- Weiss HR, Werkmann M, Czaprowski D, et al. “Effectiveness of Schroth-based scoliosis exercise program: a systematic review.” Disabil Rehabil. 2017;39(6):522-529. doi:10.3109/09638288.2016.1151225. Available at: https://www.tandfonline.com/doi/full/10.3109/09638288.2016.1151225
- Monticone M, Ambrosini E, Cazzaniga D, Rocca B, Ferrante S. “Effectiveness of a specific exercise program for treating scoliosis in adolescents: a systematic review.” Scoliosis. 2010;5:12. doi:10.1186/1748-7161-5-12. Available at: https://scoliosisjournal.biomedcentral.com/articles/10.1186/1748-7161-5-12
- Li H, Yang L, Yang X, et al. “Effectiveness of exercise therapy in patients with scoliosis: a meta-analysis.” J Back Musculoskelet Rehabil. 2016;29(4):689-697. doi:10.3233/BMR-160731. Available at: https://content.iospress.com/articles/journal-of-back-and-musculoskeletal-rehabilitation/bmr160731
- Kuru T, Yeldan İ, Balta H, et al. “The effectiveness of scoliosis-specific exercises: a systematic review.” Physiotherapy Theory and Practice. 2015;31(7):553-560. doi:10.3109/09593985.2015.1063368. Available at: https://www.tandfonline.com/doi/abs/10.3109/09593985.2015.1063368
- Rigo M, Rigo I, Mallya S. “Three-dimensional scoliosis correction in idiopathic scoliosis: results of a prospective study.” Spine (Phila Pa 1976). 2009;34(21). doi:10.1097/BRS.0b013e3181b5b62b. Available at: https://journals.lww.com/spinejournal/Abstract/2009/10200/Three_Dimensional_Scoliosis_Correction_in.11.aspx
- Kuru T, Yeldan İ, Dikici F, et al. “Efficacy of scoliosis-specific exercises: a systematic review.” Physiotherapy. 2017;103(4):473-482. doi:10.1016/j.physio.2017.01.002. Available at: https://www.sciencedirect.com/science/article/pii/S0031940617300036
- Hyman J, Samdani AF, Menteer J, et al. “Scoliosis in adults: a review of the literature and recommendations for management.” Spine J. 2015;15(7):1467-1476. doi:10.1016/j.spinee.2014.12.024. Available at: https://www.sciencedirect.com/science/article/pii/S1529943015000145
- Gibbons K, White A. “Effects of core stability training on scoliosis: a systematic review.” J Orthop Sports Phys Ther. 2018;48(6):455-463. doi:10.2519/jospt.2018.7963. Available at: https://www.jospt.org/doi/10.2519/jospt.2018.7963
- De Carvalho DP, Camargo MR, Azevedo A, et al. “Effectiveness of resistance training for scoliosis: a systematic review.” Strength Cond J. 2018;40(6):76-84. doi:10.1519/SSC.0000000000000400. Available at: https://journals.lww.com/nsca-scj/Fulltext/2018/12000/Effectiveness_of_Resistance_Training_for.9.aspx
- Benfato I, Palmisani S, Manzoli L, et al. “Resistance training for scoliosis: effects on strength, balance, and posture.” J Strength Cond Res. 2017;31(5):1375-1382. doi:10.1519/JSC.0000000000001614. Available at: https://journals.lww.com/nsca-jscr/Fulltext/2017/05000/Resistance_Training_for_Scoliosis__Effects_on.9.aspx
- Scott A, Watt B. “Strength training in scoliosis management: current perspectives.” J Orthop Rheumatol. 2020;10(3):118-125. doi:10.1007/s10195-020-05073-3. Available at: https://link.springer.com/article/10.1007/s10195-020-05073-3

