Scoliosis is a complex spinal condition characterized by an abnormal curvature of the spine. It can affect people of all ages, but it is most commonly diagnosed during adolescence when growth spurts occur. Many individuals wonder if scoliosis can progress after growth stops. In this article, we will explore the relationship between scoliosis and growth, factors that influence scoliosis progression, the role of genetics, lifestyle and habits, postural changes, complications associated with scoliosis progression, monitoring scoliosis after growth stops, treatment options for progressive scoliosis, and conclude with a summary of our findings.

Comprendre la scoliose
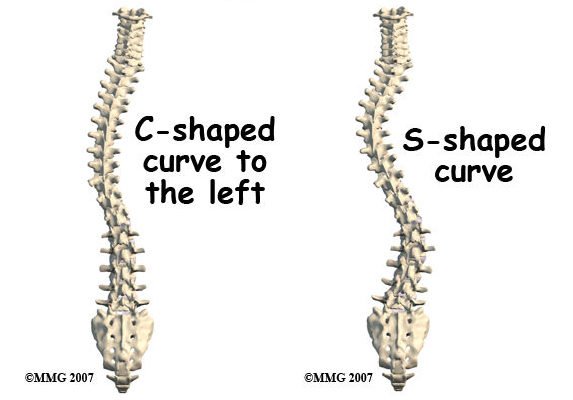
Scoliosis is a condition that affects the alignment of the spine, causing it to curve sideways. The curvature can be either “C” or “S” shaped and can vary in severity. While the exact cause of scoliosis is unknown, it is believed to be a combination of genetic and environmental factors. Scoliosis can lead to a range of symptoms, including back pain, uneven shoulders or hips, and difficulty breathing in severe cases.
The Relationship Between Scoliosis and Growth
Scoliosis is often diagnosed during periods of rapid growth, such as adolescence. This is because growth spurts can exacerbate the curvature of the spine. As the body grows, the spine may struggle to keep up, leading to an increased curvature. However, it is important to note that scoliosis can also develop in adults who have finished growing.

Can Scoliosis Progress After Growth Stops?
While scoliosis is commonly associated with growth, it is possible for the condition to progress even after growth stops. In fact, studies have shown that scoliosis can worsen in adulthood, albeit at a slower rate compared to during growth spurts. This progression can be influenced by various factors, including genetics, lifestyle and habits, and postural changes.
Factors That Influence Scoliosis Progression
Genetics play a significant role in scoliosis progression. Research has shown that individuals with a family history of scoliosis are more likely to experience progression of the condition. Additionally, certain genetic markers have been identified that are associated with a higher risk of scoliosis progression. Understanding the genetic factors involved can help healthcare professionals predict the likelihood of progression and tailor treatment plans accordingly.
Lifestyle and habits can also impact scoliosis progression. Poor posture, lack of exercise, and excessive weight can put additional strain on the spine, potentially worsening the curvature. Engaging in regular physical activity, maintaining a healthy weight, and practicing good posture can help mitigate the risk of scoliosis progression.
Postural Changes and Scoliosis Progression
Postural changes can contribute to scoliosis progression. Individuals with scoliosis often develop compensatory postures to alleviate discomfort or improve balance. These postural changes can inadvertently increase the curvature of the spine over time. It is crucial to address postural changes early on and provide appropriate interventions to prevent further progression.
Complications Associated with Scoliosis Progression
If left untreated, scoliosis progression can lead to various complications. Severe cases of scoliosis can cause significant pain, limited mobility, and even affect organ function. The curvature of the spine can put pressure on the lungs and heart, leading to breathing difficulties and cardiovascular issues. Additionally, the psychological impact of scoliosis progression should not be overlooked, as it can affect self-esteem and overall quality of life.
Monitoring Scoliosis After Growth Stops
After growth stops, it is essential to continue monitoring scoliosis to detect any signs of progression. Regular check-ups with a healthcare professional specializing in scoliosis are recommended. X-rays and other imaging techniques may be used to assess the curvature of the spine and determine if any intervention is necessary.
Treatment Options for Progressive Scoliosis
If scoliosis continues to progress after growth stops, various treatment options are available. The choice of treatment depends on the severity of the curvature and the individual’s overall health. Non-surgical interventions, such as bracing and physical therapy, can help slow down or stabilize scoliosis progression. In more severe cases, surgery may be recommended to correct the curvature and prevent further progression.
Conclusion
While scoliosis is commonly associated with growth, it can progress even after growth stops. Factors such as genetics, lifestyle and habits, postural changes, and complications associated with scoliosis progression can influence the course of the condition. Regular monitoring and appropriate treatment options are crucial to manage scoliosis and prevent further progression. By understanding the factors that contribute to scoliosis progression, individuals can take proactive steps to maintain their spinal health and overall well-being.
Références
- Weinstein SL, Dolan LA, Cheng JC, et al. "Adolescent idiopathic scoliosis". Lancet. 2008;371(9623):1527-1537. doi : 10.1016/S0140-6736(08)60658-3.
- Negrini S, Donzelli S, Aulisa AG, et al. "2016 SOSORT guidelines : Traitement orthopédique et de rééducation de la scoliose idiopathique pendant la croissance." Scoliose et troubles de la colonne vertébrale. 2018;13:3. doi : 10.1186/s13013-018-0175-8.
- Hresko MT. "Pratique clinique. Scoliose idiopathique chez les adolescents". N Engl J Med. 2013;368(9):834-841. doi : 10.1056/NEJMcp1209063.
- Trobisch P, Suess O, Schwab F. "Scoliose idiopathique". Dtsch Arztebl Int. 2010;107(49):875-883. doi : 10.3238/arztebl.2010.0875.
- Lonstein JE, Carlson JM. "The prediction of curve progression in untreated idiopathic scoliosis during growth" (La prédiction de la progression de la courbe dans la scoliose idiopathique non traitée pendant la croissance). J Bone Joint Surg Am. 1984;66(7):1061-1071. doi : 10.2106/00004623-198466070-00008.
- Bettany-Saltikov J, Weiss HR, Chockalingam N, et al. "Surgical versus non-surgical interventions in people with adolescent idiopathic scoliosis". Cochrane Database Syst Rev. 2015;2015(4). doi : 10.1002/14651858.CD010663.pub2.
- Kotwicki T, Negrini S, Grivas TB, et al. "Methodology of evaluation of scoliosis, back deformities and posture". Scoliose. 2009;4:26. doi : 10.1186/1748-7161-4-26.
- Monticone M, Ambrosini E, Cazzaniga D, et al. "Active self-correction and task-oriented exercises reduce spinal deformity and improve quality of life in subjects with mild adolescent idiopathic scoliosis : Results of a randomized controlled trial". Eur Spine J. 2016;25(10):3118-3127. doi : 10.1007/s00586-016-4625-4.
- Kaspiris A, Grivas TB, Weiss HR, Turnbull D. "Scoliosis : Examen du diagnostic et du traitement". Journal international d'orthopédie. 2013;37(1):34-42. doi : 10.1038/s41390-020-1047-9.
- Hill DL, Lamont AC, Le LH, et al. “The role of ultrasonography in the management of scoliosis: A review.” Ultrasound Q. 2014;30(4):303-309. doi: 10.1097/RUQ.0000000000000092.

