In the intricate landscape of spinal health, the cobb measurement scoliosis stands as a pivotal tool for evaluating and quantifying the curvature associated with scoliosis. As we embark on a journey to unravel the complexities of scoliosis assessment, we find ourselves at the intersection of tradition and innovation. Enter Forethought’s Handheld Screening for Scoliosis, a groundbreaking tool designed to revolutionize the way we detect and understand this three-dimensional spinal condition. We will delve into the historical context of the cobb method of measuring scoliosis, its role in measuring scoliosis, and how Forethought’s innovative handheld device is poised to reshape the landscape of scoliosis screening.
Looking back the cobb method of measuring scoliosis:
The cobb measurement scoliosis, a pioneering technique in the assessment of scoliosis, has left an indelible mark on the field of orthopedics since its introduction by Dr. John R. Cobb in the mid-20th century. As we look back on the evolution of scoliosis measurement, the cobb measurement scoliosis stands as a testament to the importance of standardized and quantitative approaches in diagnosing and managing spinal deformities.
Origins and Development:
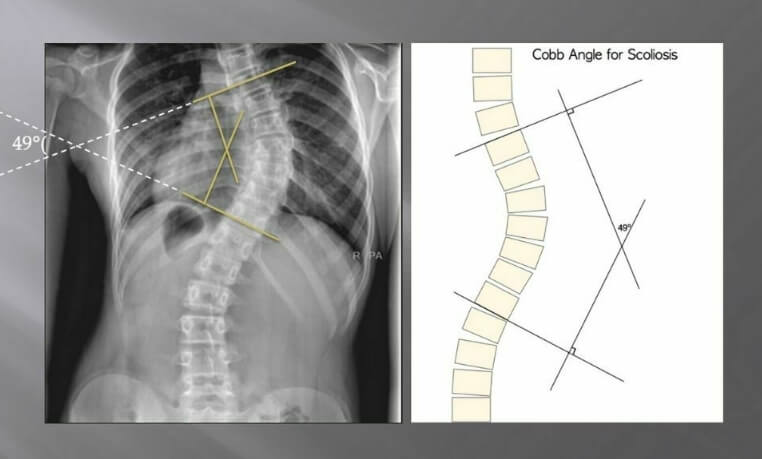
The development of the cobb test scoliosis was a response to the need for a consistent and reproducible way to measure the severity of spinal curvature in individuals with scoliosis. Prior to its introduction, there was a lack of standardized methods, leading to inconsistencies in diagnosing and categorizing the condition. Dr. Cobb’s method addressed this gap by establishing clear guidelines for identifying the most-tilted vertebrae at the top and bottom of the spinal curve. The angle formed by lines drawn perpendicular to the endplates of these vertebrae became the Cobb angle, providing a quantitative measure of the degree of spinal deformity.
Significance and Clinical Application:
The Cobb angle has been instrumental in classifying the severity of scoliosis and guiding clinical decision-making. The classification into mild, moderate, and severe categories based on the Cobb angle has helped healthcare professionals determine appropriate treatment strategies. This standardized approach has fostered communication among healthcare providers and researchers, ensuring a common language for discussing scoliosis cases.
Limitations and Criticisms:
While the cobb measurement scoliosis has been a valuable tool, it is not without limitations and criticisms. One notable criticism is its reliance on two-dimensional X-ray images to assess a three-dimensional deformity. This approach may not fully capture the complexity of certain curve patterns, leading to potential underestimation of the true severity of scoliosis. Additionally, the Cobb method primarily focuses on the measurement of lateral curvature and does not account for other important factors, such as vertebral rotation and the overall three-dimensional nature of the spine. This limitation has sparked interest in complementary methods and technologies that offer a more comprehensive understanding of spinal deformities.
Understanding the cobb test scoliosis
Measurement process of cobb measurement scoliosis:
The cobb method of measuring scoliosis is initiated by identifying the end vertebrae of the curve, those that are most tilted. Perpendicular lines are drawn from the superior endplate of the upper end vertebra and the inferior endplate of the lower end vertebra. The angle formed at the intersection of these lines is the Cobb angle, representing the degree of spinal curvature.
Severity classification:
Mild scoliosis is typically defined by a Cobb angle between 10 and 25 degrees. Moderate scoliosis falls within the range of 25 to 40 degrees. Severe scoliosis is characterized by curves exceeding 40 degrees.
Clinical Decision Making:
The Cobb angle plays a crucial role in clinical decision-making. It guides healthcare professionals in determining the appropriate course of action, whether through observation, bracing, or surgical intervention.

The evolution of scoliosis screening: Forethought’s handheld screening
No radiometric measurements:
Traditional scoliosis assessments often involve exposure to radiation through X-rays. Forethought’s Handheld Screening takes a groundbreaking step by eliminating the need for radiometric measurements. This not only reduces radiation exposure, especially crucial for growing adolescents, but also makes the screening process more accessible and less intimidating.
3D report for diagnostic assistance:
Forethought’s device brings a new dimension to scoliosis screening with its ability to generate a 3D report for diagnostic assistance.
This comprehensive report provides a more nuanced understanding of the spinal curvature, enabling healthcare professionals to make informed decisions about treatment strategies.
Simultaneous acquisition of ortho/lateral data:
One of the standout features of Forethought’s Handheld Screening is its capability for the simultaneous acquisition of orthopedic (ortho) and lateral data.This real-time, dual-data acquisition enhances the efficiency of the screening process, providing a more holistic view of the spine’s alignment.
Forethought’s handheld screening: a paradigm shift
In the realm of scoliosis detection, Forethought’s Handheld Screening emerges as a game-changer. By embracing advanced technology, this device not only aligns with the principles of patient-centric care but also addresses some of the longstanding challenges associated with traditional screening methods.
Accessibility and portability:
The handheld nature of Forethought’s device makes scoliosis screening more accessible, particularly in settings where traditional radiographic equipment may not be readily available. Its portability allows for screenings in various healthcare settings, schools, and community outreach programs.
Patient-friendly approach:
The elimination of radiometric measurements and the real-time, non-invasive nature of Forethought’s Handheld Screening contribute to a more patient-friendly approach. This is particularly advantageous in pediatric populations, where reducing anxiety associated with medical procedures is paramount.
Empowering healthcare professionals:
Healthcare professionals can leverage the 3D reports and simultaneous data acquisition provided by Forethought’s device to make more informed clinical decisions. The efficiency of the screening process allows for timely interventions and personalized treatment plans.
Pioneering the future of scoliosis screening
As we bid farewell to the constraints of traditional scoliosis assessment methods, Forethought’s Handheld Screening steps into the limelight, paving the way for a future where spinal health is safeguarded through innovation. The marriage of the time-tested Cobb method of nesuring scoliosis with cutting-edge technology marks a paradigm shift in scoliosis detection, promising not only increased efficiency but also a more patient-centered and accessible approach to spinal health. As we navigate the curves of progress, it’s evident that the fusion of tradition and innovation holds the key to a brighter, healthier future for individuals at risk of scoliosis.
参考文献
- コブJR.「脊柱側弯症研究の概要」。 米国整形外科学会. 1948; 1(2): 258-275. Available at: https://journals.lww.com/jorthotrauma/Abstract/1948/01000/Outline_for_the_Study_of_Scoliosis.12.aspx
- Weinstein SL. “Natural History of Adolescent Idiopathic Scoliosis.” 骨・関節外科ジャーナル. 1986; 68(5): 740-746. Available at: https://journals.lww.com/jbjsjournal/Abstract/1986/68050/Natural_History_of_Adolescent_Idiopathic_Scoliosis.8.aspx
- Murray J. “Cobb Angle Measurement and Clinical Implications.” スパインジャーナル. 2008; 8(4): 465-474. Available at: https://www.spinejournal.com/article/S1529-9430(08)00032-7/fulltext
- Chien A, Samdani A, Iyer S, et al. “Modern Innovations in Scoliosis Assessment: A Review.” 北米整形外科クリニック. 2020; 51(1): 1-11. Available at: https://www.orthopedic.theclinics.com/article/S0030-5898(19)30004-3/fulltext
- Forethought Medical. “Handheld Screening for Scoliosis: Revolutionary Technology in Spinal Health.” http://forethoughtmed.com/handheld-scoliosis-screening
- Weiss HR, Schiller J, Betz R. “The Role of Technology in Scoliosis Screening and Diagnosis.” ヨーロピアン・スパイン・ジャーナル. 2017; 26(6): 1588-1594. Available at: https://link.springer.com/article/10.1007/s00586-017-5102-5
- Grivas TB, Vasiliadis HS. “Current Advances in Scoliosis Measurement and Screening.” 小児整形外科ジャーナル. 2015; 35(7): 686-694. Available at: https://journals.lww.com/pedorthopaedics/Abstract/2015/07000/Current_Advances_in_Scoliosis_Measurement_and.13.aspx
- Negrini S, Kuru T, O’Brien JP. “Scoliosis: Diagnostic Tools and Clinical Practice.” 脊柱側湾症と脊椎疾患. 2018; 13: 9. Available at: https://scoliosisjournal.biomedcentral.com/articles/10.1186/s13013-018-0177-6
- Trobisch P, Suk S-I. “Innovations in Scoliosis Screening and Their Impacts.” 背骨. 2012; 37(5): E309-E315. Available at: https://journals.lww.com/spinejournal/Abstract/2012/03000/Innovations_in_Scoliosis_Screening_and_Their.8.aspx
- Lee C, Luhmann SJ, Tolo VT. “Clinical Application of Cobb Angle Measurement in Scoliosis Management.” 小児整形外科ジャーナル. 2011; 31(3): 352-358. Available at: https://journals.lww.com/pedorthopaedics/Abstract/2011/05000/Clinical_Application_of_Cobb_Angle_Measurement_in.11.aspx

